
Originally due to take place in Paris, France, the 6th Congress of the European Academy of Neurology (EAN) was held virtually - for the first time in its history - as a result of the COVID-19 pandemic.

Professor Claudio Bassetti, Acting President of the EAN
More than 16,000 participants registered to take part in the EAN Virtual Congress, doubling the previous number of attendees and making it the biggest virtual neurology meeting to date. The overarching theme for this year’s pioneering meeting was “Time for Action - Predict, Prevent, Repair”. All major neurological diseases and disorders were covered in a state-of-the-art online scientific programme, with a focus on multiple sclerosis (MS), epilepsy, stroke, headache, dementia, movement disorders and musculoskeletal disorders. This report covers the therapy areas of MS, Alzheimer’s disease, and Huntington’s disease.
The COVID-19 pandemic has imposed an incredible health, emotional and economic burden on society and, while difficult times require creative and courageous solutions, they can also open up new opportunities and avenues to a brighter future, said Acting EAN President, Professor Claudio Bassetti. We must stay positive, strong and more united than ever to overcome this crisis, Professor Bassetti insisted.
“We cannot stop the spread of the virus but what we can do is prevent it from interrupting scientific exchange and learning within our neurology community.”
Professor Claudio Bassetti
Table of Contents
Multiple Sclerosis
Practical Guidelines to Assess MRI Lesions that are Typical or Atypical for MS
Key changes to the 2017 McDonald criteria for DIS and DIT
Promoting Structural Repair and Functional Recovery in MS
Ongoing and future therapeutic strategies
Multiple sclerosis, differential diagnosis: Neuro-Ophthalmological Mimickers
Multiple sclerosis: Pregnancy in Neurological Disorders
How to Handle Safety Issues in MS Treatment
Autonomic Nervous System Dysfunction In MS: Highlight Session
Alzheimer’s Disease and Dementia
Neuroimaging in Dementia: News and Perspectives
Huntington's Disease
Differential Diagnosis and Therapy of Movement Disorders for General Neurologists
Multiple Sclerosis
Practical Guidelines to Assess MRI Lesions that are Typical or Atypical for MS
The goal of this case-based workshop was to reinforce the correct recognition of MS lesions included in 2017 McDonald diagnostic criteria, focusing on both typical magnetic resonance imaging (MRI) features and “red flags” suggestive of an alternative diagnosis.
Typical MS lesions were reviewed by Celine Louapre, Paris, France, who used two clinical case studies and multiple MRI images to illustrate the characteristic periventricular, cortical/juxtacortical, infratentorial and spinal cord lesions associated with MS. She reminded delegates that MS enacts multifocal and chronic neurological damage which is typified by both dissemination in space (DIS) and dissemination in time (DIT). MRI remains ‘the’ tool for diagnosing MS, said Dr Loupare, and offers excellent sensitivity assuming clinicians have the experience to recognise MS-type lesions correctly. Sensitivity can be boosted by increasing the resolution (to 3T or 7T) or improving the sequences, for example, using short T1 inversion recovery (STIR) for imaging the spinal cord and double inversion recovery (DIR) for cortical lesions.
Key changes to the 2017 McDonald criteria for DIS and DIT
Using clinical cases as examples, Christian Enzinger, Graz, Austria, outlined practical guidelines for the assessment of typical and atypical MS lesions, including how to distinguish MS from other key demyelinating disorders.
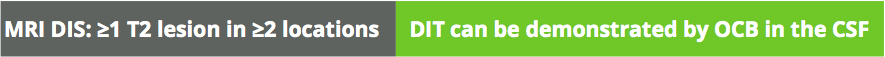
CSF, cerebrospinal fluid; DIS, dissemination in space; DIT, dissemination in time; OCB, oligoclonal bands
How to distinguish MS from other demyelinating disorders
Dr Enzinger emphasised that MRI scans must always be interpreted in the appropriate clinical context and grounded in the basic knowledge of what constitutes a lesion. The integration of history, examination, MRI and laboratory evidence by a clinician with MS-related expertise remains fundamental to the reliable diagnosis of MS or alternative conditions. In cases with lingering uncertainty, the threshold for carrying out additional tests should be low, said Dr Enzinger, and should include spinal cord MRI and/or cerebrospinal fluid (CSF) examination.
Cristina Granziera, Basel, Switzerland, gave a masterclass on how to decipher “red flags” suggestive of central nervous system (CNS) vasculitis and other inflammatory disorders. Dr Granziera highlighted the MIMICS algorithm as a key tool for identifying atypical MS lesions in everyday clinical practice. The central vein sign and iron rims can also provide potentially valuable clues in the differential diagnosis of MS, particularly in distinguishing from other CNS inflammatory vasculopathies.

DIS, dissemination in space; NMOSD, neuromyelitis optica spectrum disorder
Differential diagnosis of MS using the MIMICS algorithm
Promoting Structural Repair and Functional Recovery in MS
Promoting CNS remyelination and neuroprotection are critical to the prevention of disability progression in MS. This symposium explored underlying mechanisms of myelin repair and evolving therapeutic strategies aimed at stimulating remyelination/neuroprotection.
The pathophysiological basis of functional recovery was discussed by Diego Centonze, Rome, Italy, who summarised existing data supporting the role of synaptic plasticity changes in the clinical compensation for structural damage in MS. He explained that clinical disability in MS appears when the long-term potentiation (LTP) reserve of surviving neurons is exhausted, and that rehabilitation exerts its clinical benefits by preserving or boosting these reserves. LTP requires the activation of a range of substances - N-methyl-D-aspartate, cannabinoids, dopamine and neurotrophins - raising the possibility that pharmacological interventions which stimulate these target receptors could enhance the effects of rehabilitation by favouring synaptic plasticity. LTP can also be impaired by acute inflammation which may further explain the beneficial impact of disease-modifying drug (DMDs) therapy in MS.

DWI, diffusion-weighted imaging; DW-MRS, diffusion-weighted magnetic resonance spectroscopy; NAA-HMRS, N-acetylaspartate H-magnetic resonance spectroscopy; MRI, magnetic resonance imaging.
Advantages and disadvantages of neuroimaging techniques
Benedetta Bodini, Paris, France, gave an overview of imaging methods used in the evaluation of remyelination and neuroprotection in MS, highlighting the advantages and disadvantages of available tools.
Dr Bodini proposed that MRI and positron emission tomography (PET) should both be employed as endpoints in Phase 2 clinical trials evaluating promyelinating and neuroprotective treatments for MS. Future outcome measures may also incorporate imaging techniques to assess the underlying mechanisms which lead to neurodegeneration.
Moving forward, Dr Bodini suggested that PET could be used to validate single MRI sequences or a combination of multiple measures to improve MRI specificity for myelin and neurons.
Ongoing and future therapeutic strategies
Gianvito Martino, Milan, Italy, delivered a cutting-edge talk on the use of neural stem cell therapy in MS. Dr Martino explained how transplanted stem cells work through a combination of both direct cell replacement and the bystander effect. They exert their neuroprotective effects by secreting trophic factors and immunomodulatory molecules that foster endogenous precursors to promote remyelination and to rescue damaged axons and neurons. Depending on the tissue microenvironment, transplanted neural precursor cells (NPCs) appear able to recapitulate the ‘physiological’ non-neurogenic homeostatic and neurogenic functions produced by endogenous NPCs. The bench-to-bedside translation of NPC transplants has already begun in MS, revealed Dr Martino, and appears safe in the first nine patients to have completed 2 years of follow-up, with no reported side-effects. Importantly, the bystander effect was measurable in the CSF as early as 3 months post-transplantation.
“In the CNS of patients transplanted with NPCs we found that, after 3 months, the microenvironment was changed from a proinflammatory to an antiinflammatory state.”
Gianvito Martino
Multiple sclerosis, differential diagnosis
Neuro-Ophthalmological Mimickers
This case-based workshop was designed to support knowledge and practice in the differential diagnosis and management of three neuro-ophthalmological conditions that commonly present to the neurologist such as MS-related acute optic neuritis.
Mimickers of MS-related acute optic neuritis were addressed by João Lemos, Coimbra, Portugal. Dr Lemos reviewed six real-world case studies, highlighting important “red flag” signs and symptoms suggestive of alternative diagnoses. Dr Lemos cautioned clinicians not to suspect MS-related optic neuritis if a patient’s history includes preceding febrile illness, absence of periocular pain, the presence of photopsias or metamorphopsia, bilateral simultaneous presentation, no improvement or severe visual loss after 3 weeks, or steroid dependency. He also highlighted key clinical clues to be alert for during examination and work-up of the patient.
Atypical features observed in an examination of MS-related optic neuritis

Atypical features observed in an examination of MS-related optic neuritis
- Extensive optic nerve enhancement or a severe loss of nerve fibre layer on optical coherence tomography (OCT), particularly if this doesn’t fit the pattern of temporal loss in MS
- The presence of subretinal fluid
- Retinal pigment epithelium disruption
All of these features should make you think of an alternative diagnosis, Dr Lemos concluded.
Multiple sclerosis
Pregnancy in Neurological Disorders
This teaching course addressed the myriad questions and issues that can arise when pregnancy occurs or becomes desirable in women with neurological disorders. Letizia Leocani, Milan, Italy, spoke about pregnancy in MS, a particularly pertinent topic given that the disease predominantly affects women of child-bearing age. Dr Leocani insisted that an MS diagnosis does not preclude pregnancy and that pregnancy should not be discouraged a priori.
However, it is important to discuss family planning early in the clinical journey and have a clear action plan for each step in advance - from pre-conception, through pregnancy and into the postpartum period. For patients with active disease already receiving DMD treatment, alemtuzumab or cladribine can be considered before pregnancy or natalizumab given during pregnancy (up to 30 weeks gestation). For the treatment of relapses during pregnancy, methylprednisolone IV is recommended and any neuroimaging should always be carried out without gadolinium. Glatiramer acetate, interferon-β and natalizumab are all suitable options for use during breastfeeding, said Dr Leocani.

When should natalizumab be stopped and restarted in patients with MS planning pregnancy?
Pregnancy planning and DMDs: Balancing risks

Balancing the risks of DMDs in patients with MS planning pregnancy
“Post-partum is the critical phase so it’s very important to consider restoring a DMD to protect against relapse over that first year which we know is associated with increased disability later on.”
Letizia Leocani
How to Handle Safety Issues in MS Treatment
Building on the key topic of safety, this teaching session reviewed strategies for mitigating and managing risks associated with powerful immunosuppressive/modulatory therapies for MS.
Ralf Gold, Bochum, Germany, examined the important safety risk posed by progressive multifocal leukoencephalopathy (PML). He pinpointed natalizumab, fumarates and fingolimod as the key DMD culprits implicated in PML, but noted that the risk with modern oral treatments remains low. According to the new risk stratification algorithm in Europe, patients on natalizumab with low anti-JC virus antibody index values and no history of prior immunosuppressant use should be retested every 6 months once they reach the 2-year treatment period. Options for countering the risk include extended-interval dosing of natalizumab, supportive measures, immune reconstitution inflammatory syndrome (IRIS) to ‘flush’ the immune system and steroids. Professor Gold also warned about the potential “spillover” scenario where PML unfolds during new follow-up medication. Aside from PML, other important sideeffects to be aware of with modern monoclonal treatments include documented cases of severe B-cell-mediated CNS diseases secondary to alemtuzumab and eosinophilic encephalomyelitis with daclizumab (now withdrawn).
How could DMDs increase infection risk in patients with MS?
The dual issues of infections and vaccinations were tackled by Lucia Moiola, Milan, Italy. Dr Moiola underscored the importance of prevention versus treatment, both for reducing infectious morbidity and mortality and avoiding interruptions to DMD therapy. Clinicians should also be equipped with an in-depth knowledge of drugs’ mode/duration of action to facilitate recognition of key infection-related adverse events and practice active pharmacovigilance. Strategies for prevention include: infection identity cards, vaccine cards and treatment of active infections. Dr Moiola stressed that vaccination is essential in MS and the timing and schedule should be tailored on an individual basis according to specific risk factors such as travel, sexual habits and employment.
Autonomic Nervous System Dysfunction In MS
Highlight Session
This symposium on the final day of EAN 2020 shone a spotlight on key developments and state of-the-art developments in the field of autonomic disorders.
Mario Habek, Zagreb, Croatia, explored the clinical implications of autonomic nervous system (ANS) dysfunction in MS, with a focus on the MS prodrome, ANS symptoms and ANS testing in MS. Dr Habek described the specific pattern of autonomic abnormalities in MS, where disease activity measured by relapses or new T2 lesions affects sympathetic parts of the ANS. In contrast, disease progression, which is the consequence of neurodegeneration, is connected to abnormalities in the parasympathetic nervous system. Dr Habek also outlined how ANS dysfunction evolves over the time course of the disease, with initial ANS symptoms appearing up to 10 years prior to MS diagnosis and accumulating increasingly as the disease advances. T2 lesion load, in particular, appears to be a key predictor of worsening composite autonomic severity score.
ANS symptoms in the MS prodrome

ANS symptoms in the MS prodrome
Director of the German Aerospace Centre - Jens Jordan, Cologne, Germany - gave an intriguing presentation on the relevance of autonomic space medicine to daily clinical neurology, applying lessons learnt in astronauts to patients on earth. One of the key insights gained from studying astronauts is how the ANS adapts in order to maintain physiology. Orthostatic symptoms result from the interaction of the nervous system and other mechanisms, with volume regulation proving particularly important. The ability to stand and maintain blood pressure can also be lost; ‘use it or lose it’, Dr Jordan warned.
“Space research can drive new technology which may have utility for patients on earth, particularly those suffering from autonomic nervous system disease”
Jens Jordan
Gregor Wenning, Innsbruck, Austria, discussed developments in DMDs for multiple systematrophy (MSA), a progressive neurological disorder which has some overlapping clinical signs and symptoms with MS. Dr Wenning gave an overview of the large number of DMD candidates currently in the clinical pipeline. Broadly speaking, there are two key targets for DMDs in MSA: reduction of α-synuclein deposits and inhibition of neuroinflammation/microglial activation. Although a number of Phase 3 therapeutic trials have already beencompleted with agents such as rifampicin, riluzole (indicated for amyotrophic lateralsclerosis) and minocycline, results were predominantly negative. Looking ahead, Dr Wenning highlighted the iron chelator PBT434 and the α-synuclein oligomerisation inhibitoranle138b as the most promising of the current early-stage drugs while, among the moreclinically advanced candidates, positive results have been attained with mesenchymal stemcells and epigallocatechin gallate.
Alzheimer’s Disease and Dementia
Neuroimaging in Dementia: News and Perspectives
Structural and functional neuroimaging biomarkers play a key role in the clinical diagnosis of diseases that cause cognitive impairment. This focused workshop session explored new approaches - based on the stalwarts of MRI and PET - which are being explored for the neuroimaging of dementing disorders.
Massimo Filippi, Milan, Italy, reviewed new and established MRI tools in cognitive disorders, looking at what is consolidated, nearly consolidated and new in the field.
What is consolidated and new in MRI?
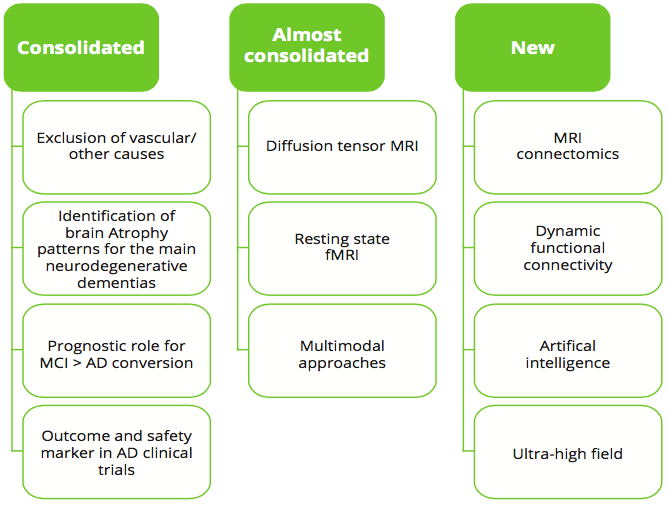
What is consolidated and new in neuroimaging in patients with dementia?
Structural MRI is mandatory to exclude the presence of secondary causes and also helps clinicians visualise the topography of atrophy, which can shed light on the underlying neurodegenerative aetiology. Dr Filippi stressed that MRI is ‘more than hippocampal volume’, with strong utility in the differential diagnosis of Alzheimer’s disease (AD) versus non-AD dementia and also a useful prognostic indicator in mild cognitive impairment (MCI). Advanced techniques are already able to measure white matter and resting state functional MRI (fMRI) changes. Looking to the future, higher resolution imaging such as 7T will allow for increasingly detailed, cortical layer-specific analysis of microcircuits implicated in the earliest stages of disease.
“The future role for MRI includes complex mathematical and technological approaches that integrate and optimise available data."
Massimo Filippi
The impact of amyloid and tau PET in the diagnosis and prognosis of neurodegenerative diseases was examined by Alexander Drzezga, Cologne, Germany. Amyloid PET is a clinically available method that may facilitate the very early diagnosis of amyloid pathology (although time to conversion in healthy participants without cognitive symptoms remains unclear), with additional prognostic value in MCI and subjective cognitive decline. Its differential diagnostic power covers detection of atypical AD and exclusion of pseudo-AD, but it is not yet a reliable tool for staging. Tau-PET - although still experimental - also offers a window into early diagnosis at the start of neurodegeneration, albeit with less sensitivity in the preclinical stages of disease. Diagnostically, it can discriminate between tau-negative versus tau-positive forms of dementia, with the deposition pattern a key delineating factor, and also shows value as a tool for staging and follow-up. Dr Drzezga advised that the ultimate choice between amyloid or tau-PET should depend on the diagnostic question, with a combination of the two biomarkers likely to prove most helpful with regards to ATN classification framework (A stands for β-amyloid [Aβ] pathology, T for tau pathology and N for other non-specific biomarkers of neurodegeneration).
“Tau-PET allows us to see where the neurodegeneration is ongoing and what is underlying it - so it’s a useful tool that integrates a lot of information via a single imaging modality”
Alexander Drzezga
Role of tau imaging

Role of tau imaging in patients with dementia
‘What can we learn from discordant PET and CSF biomarkers?’ asked Femke Bouwman, Amsterdam, the Netherlands, in a presentation which reviewed key amyloid and tau biomarkers in AD and their relation to neuropathology. CSF and PET represent different biomarker modalities for measuring AD pathology and any discordance can shed light on the underlying pathological changes. CSF biomarker abnormality precedes PET biomarker abnormality for both amyloid and phosphorylated tau (p-tau), while combined CSF and PET abnormality (i.e. concordance) precludes progressive cognitive decline in both prodromal and dementia stages. Dr Bouwman stressed that, in cases where biomarkers are discordant, it is important to consider other neurodegenerative diseases. Moving forward, more neuropathologically-specific biomarkers are urgently needed to unravel the complex multiple pathology of neurodegeneration, Dr Bouwman concluded.
Fluid and Structural Disease Biomarkers to Predict Neurodegenerative Diseases
This workshop session focused on the benefits of integrated translational and clinical research, showcasing a series of biomarkers that may enable the prediction of disease onset and preventive therapeutic intervention in neurodegenerative diseases.
Mathias Junker, Tubingen, Germany, explored the possibility of bridging the translational gap using murine models of neurodegenerative diseases, which he described as ‘wonderful tools’ for predicting and understanding fluid changes in the clinical setting. Thanks to these murine studies, we now know that both CSF tau (and p-tau) levels are tightly correlated to Aβ aggregation, said Dr Junker. Neurofilament light (NFL) levels in both the CSF and blood also afford a reliable marker for neurodegeneration associated with proteopathic lesions in the brain. Remarkably, the rate of change in NFL levels has been shown to predict cortical thinning and cognitive changes up to 16 years before the expected onset of typical AD symptoms.
“We are now at the stage where pre-symptomatic biomarker changes in AD are becoming so important some people think we should screen the entire population. But before we can move in that direction we must know more about what they are telling us mechanistically…”
Mathias Junker
CSF and blood-based disease, treatment response biomarkers in AD and other neurodegenerative disorders were discussed by Charlotte Teunissen, Amsterdam, the Netherlands. She noted that biomarker panels are vital for the differential diagnosis of different dementias and there is an urgent need to develop new biomarkers, particularly for microglia and astrocytic activity. Ongoing research efforts in the biomarker arena include bPRIDE, a Europe-wide initiative using different multi-marker blood proteins panels for the early discrimination of dementias. Dr Teunissen explained that plasma panels of amyloid, p tau, NFL and glial fibrillary acidic protein can be robustly analysed using ultrasensitive technologies and are likely to be used across AD prescreening, diagnosis and therapy response monitoring in the near future.
Federica Agosta, Milan, Italy, gave a talk covering structural and functional markers of neurodegeneration with applicability across both preclinical and clinical disease stages. She outlined the biomarker-based framework for AD which classifies imaging markers as either diagnostic or progression. In AD, imaging is very powerful for detecting progression markers of neuronal injury using tools such as fluorodeoxyglucose (FDG) PET, MRI and CSF t-tau, alongside newer modalities like diffusion tensor imaging (DTI) and resting-state fMRI. Moving forward, it may even prove possible to predict the network-dependent spread of pathology in neurodegenerative diseases, said Dr Agosta, with several studies now underway in this exciting area.
“The pathology in neurodegenerative conditions may spread from one region to another through connectivity, with the structural architecture of the brain able to modulate this progression”
Federica Agosta

Diagnostic and progression imaging biomarkers in neurodegenerative disorders: key features
Huntington's Disease
Differential Diagnosis and Therapy of Movement Disorders for General Neurologists
This teaching course set out to refresh neurologists’ knowledge of hyperkinetic movement disorders encountered in general practice such as Huntington’s disease, and bring neurologists up to speed with recent developments in the field.

Huntington’s disease currently ranks as the third most common inherited neurological disease
Susanne Schneider, Munich, Germany, provided an overview of Huntington’s disease and other choreas, which can be classified according to age of onset, time course and disease progression, distribution and aetiology (hereditary versus acquired). Alterations of fine motor tasks in Huntington’s may premanifest up to 10 years before overt disease onset and correlate with loss of corticostriatal connectivity and striatal atrophy. In addition to an ever-expanding repertoire of biomarkers, several therapeutic clinical trials for Huntington’s disease are also ongoing or in the pipeline. Candidates include antisense oligonucleotides, small molecules and microRNAs which exert their effects though mechanisms such as DNA targeting, posttranscriptional modifications to lower Huntingtin levels and methods to clear the protein. Although Huntington’s disease currently ranks as the third most common inherited neurological disease, Dr Schneider also cautioned clinicians to be aware of Huntington’s phenocopies - of which the two most common in Europe are SCR17 and chromosome 9 open reading frame 72 (C9orf72).
“These are exciting times because there are new approaches with various compounds in the pipeline for Huntington’s and clinical trials are already ongoing. The idea is to target the disease pathogenesis proximally rather than simply providing symptomatic treatment.”
Susanne Schneider
EAN President Prof Bassetti has pledged his hope for this meeting to return in physical form next year, with the 7th Congress of the EAN scheduled to take place in Vienna from the June 19–22, 2021. However, with a commitment to continued innovation and a reduction in carbon footprint, key elements from this first ever virtual congress will be retained in 2021, including online presentations and livestream sessions providing accessibility to delegates from across the globe.
©Springer Healthcare 2020. This content has been independently selected and developed by Springer Healthcare and licensed by Roche for Medically. The topics covered are based on therapeutic areas specified by Roche. Inclusion or exclusion of any product does not imply its use is either advocated or rejected. Use of trade names is for product identification only and does not imply endorsement. Opinions expressed do not reflect the views of Springer Healthcare. Springer Healthcare assumes no responsibility for any injury or damage to persons or property arising out of, or related to, any use of the material or to any errors or omissions. Please consult the latest prescribing information from the manufacturer for any products mentioned in this material.