
The 20th congress of the European Society of Retina Specialists (EURETINA) - and the society’s first ever-virtual meeting - took place between 2nd and 4th October 2020. Welcoming delegates to the congress, President Frank Holz, Germany, explained that EURETINA 2020 Virtual would feature four channels of livestreamed scientific content curated by world-renowned leaders in the field of retinal diseases. The meeting consisted of a total of 50 scientific sessions, including keynote lectures, international symposia and instructional courses.

“The worldwide upheaval due to SARSCoV-2 has starkly affected how we conduct our professional development. We know that EURETINA plays an important role in this development and as such we have been committed to pursing the society’s goals to pioneer education and to support research in the field of retina, irrespective of the challenging environment in which we now find ourselves.”
Frank Holz, University Eye Hospital Bonn, Germany
Keynote: Gisbert Richard Lecture
‘The restless fight against inherited blindness’ was the title for this year’s Gisbert Richard lecture delivered by Stanislao Rizzo, Italy. Retinal dystrophies are characterised by both genotypic and phenotypic variability, with 30% of causative genetic mutations still unknown. Prof Rizzo outlined four key stages in retinitis pigmentosa (RP) and four different therapeutic strategies to tackle them. Pharmacological treatment approaches include antioxidant, anti-apoptotic and neurotrophic agents. In the field of ocular gene therapy, 2017 marked a milestone moment when the FDA approved the first ever vision-restoring gene therapy for a cause of retinal blindness (RPE65 mutations). For patients at the advanced and end stages of RP, stem cell transplantation is a promising approach and visual prostheses can provide benefit in cases of severe vision loss where other medical options are lacking. Prof Rizzo highlighted the NR600 Nano Retina system, which incorporates 3D-neural interface technology, as a particularly promising advance in the field and noted that we are entering ‘an exciting time in the care of patients with inherited retinal diseases’.

There are different therapeutic strategies for different stages of retinitis pigmentosa
“With an estimated 36 million and growing number of blind individuals, the significance of a cure for blindness is clear and increasing.”
Stanislao Rizzo, Rome, Italy

Elisabetta Pilotto, Italy reviewed retinopathy in type 1 diabetic (T1DM) children which is associated with pathophysiological changes to retinal vessels, glial cells and neuronal cells. Diabetic retinopathy (DR) in T1DM children is characterised by very early diffuse retinal involvement and retinal flow changes, with differential involvement of the retinal plexuses. Developments in retinal imaging systems are helping to advance the role of biomarkers in defining early DR. However, Dr Pilotto cautioned that in some cases optical coherence tomography (OCT) and OCT angiography (OCTA) findings can be controversial, influenced by factors such as age of the studied population, T1DM duration and the type of analysis software used.
Amani Fawzi, USA explained how new imaging techniques have provided insights into retinal blood flow in DR, with differing effects seen in the superficial, middle and deep capillary networks. Emerging evidence indicates that an early increase in blood flow occurs before the development of DR. Blood flow then decreases with the onset of DR, an effect which appears more prominent in deep layers on OCTA. Large vessel tortuosity acts as a marker of retinopathy activity, with pan-retinal photocoagulation (PRP) producing both a reversal of tortuosity and an increase in macular blood flow.
“This is a vicious cycle where the ischaemic outer retina calls for more VEGF which in turn leads to dilation of the superficial capillary plexus (SCP).”
Amani Fawzi, Evanston, USA
Addressing the subject of deferred laser in diabetic macular oedema (DME), Michel Paques, France, questioned whether we should follow the Early Treatment Diabetic Retinopathy Study (ETDRS) guidance or look for telangiectatic capillaries (TelCaps)? TelCaps are capillary microaneurysms commonly observed in retinal vascular disease. Grid laser was the predominant treatment option for DME until the 2000s when it was superseded by anti-VEGF/steroids as first-line therapy. Identifying TelCaps may have the potential to change practice by encouraging more personalised, cost-effective management of DME; for example, using indocyanine green (ICG) staining to guide targeted laser treatment. Dr Pagues explained that his current approach is to search for and treat TelCaps in cases of circinate exudates and persisting focal oedema after a series of intravitreal injections (IVI). Moving forward, clinical trials such as the ongoing TalaDME study are needed, together with dedicated diagnostic and therapeutic protocols.

Diagnosis of TelCaps
Neil Bressler, USA discussed current and future Diabetic Retinopathy Clinical Research Network (DRCRnet) protocols. Based on insights from existing DRCRnet protocols, he outlined how baseline visual acuity (VA) can guide treatment in eyes with centre-involved DME in three scenarios. For patients with VA 20/25 or better, Protocol B of the DRCRnet showed that none of the three treatment approaches (anti-VEGF, focal/grid laser or observation) proved superior in terms of vision outcomes at 2 years and most eyes did not require rescue with anti-VEGF. For patients with VA between 20/32 to 20/40, Protocol B revealed a greater improvement in OCT thickness with aflibercept and ranibizumab compared to bevacizumab, but this did not translate into significant changes in VA. For the baseline scenario where VA was 20/50 or worse, Protocol I did reveal a difference depending on the anti-VEGF used. Aflibercept proved superior to its two counterparts in terms of VA at year 1 and 2, an outcome which Dr Bressler described as ‘clinically relevant’.
When to pursue surgical solutions for DR was discussed by Alistair Laidlaw, UK. Reactive indications for diabetic vitrectomy include vitreous haemorrhage, macular traction and tractional DME. More proactive indications which are less proven include extensive neovascularization despite laser and DME. Overall, Dr Laidlaw described diabetic vitrectomy as a common and relatively safe procedure.
Age-related macular degeneration (AMD)
Dr Klaver presented new insights into retinal disease from the EyeRisk consortium which examined 20 epidemiological studies involving 53,000 patients.

Insights provided from EyeRisk
Adnan Tufail, UK described OCT as a feature-rich modality which lends itself perfectly to the artificial intelligence (AI) based search for AMD biomarkers. AI biomarker detection is rapidly evolving and has a role in population studies and clinical trials. The ultimate aim is to obtain quantitative biomarkers able to guide therapeutic interventions and monitor response to treatment.
Robyn Guymer, Australia discussed approaches to slow the progression of intermediate AMD, focusing on the potential role of new subthreshold laser modalities. The randomised, multicentre, LEAD study (NCT01790802) showed no difference in progression rate to late AMD for nanosecond laser (2RT) treatment versus sham. However, post-hoc analysis revealed a potential impact in intermediate AMD cases without coexistent reticular pseudodrusen (RPD). Dr Guymer described these results as ‘intriguing’ and worthy of further evaluation.
“Now that we have potentially new ways of classifying earlier stages of AMD severity and progression, using multimodal imaging, it is hoped there will be a large increase in clinical trial activity investigating novel interventions in the early stages of AMD before the onset of vision-threatening complications.”
Robyn Guymer, Melbourne, Australia
Novel therapeutic approaches in neovascular AMD (nAMD) were reviewed by Jordi Mones, Spain. He highlighted three promising intravitreal drugs: brolucizumab, faricimab and KSI-301. A port delivery system (PDS) intraocular device (Roche; NCT03677934/NCT03683251) is also on the cusp of regulatory filing in the US and Europe. In the field of gene therapy, both subretinal and intravitreal approaches are being pursued (e.g. ADVM-022 and RGX314).

Pipeline therapies for nAMD
Carl Regillo, USA presented results from the Phase 3 ARCHWAY study (NCT03677934) which compared long-acting ranibizumab delivered via PDS to monthly dosing. PDS proved non-inferior and equivalent to monthly ranibizumab for change in BCVA score at weeks 36/40 - meeting the trial’s primary endpoint. Retinal thickness was controlled and PDS showed a favourable risk-benefit profile with reduction in treatment burden. Notably, 98% of patients did not require supplemental treatment before their first refill-exchange.
“With these long-acting therapies we can now be more ambitious in aiming to provide vision to our patients for 10 years or more.”
Jordi Mones, Barcelona, Spain
Dr Loewenstein discussed the potential impact of remote home OCT monitoring in AMD, which is particularly pertinent in light of the ongoing COVID-19 pandemic. The Notal OCT study showed good usability and image quality with home OCT, with around 90% of eyes successfully self-imaged by elderly AMD patients. Dr Loewenstein concluded that teleconnected OCT in patient homes has the potential to support current retina disease management as well as any future evolution which may occur in monitoring patterns, drug selection and dosing and patient outcomes.
Retinal Vascular Diseases
Reiner Schlingemann, the Netherlands, examined new insights in the pathophysiology of DME in vein occlusion. Evidence indicates that transcellular transport of proteins drives oedema formation at the inner blood-retinal barrier and that Tie-2/angiopoeitins may provide new targets for barrier restoration. In some patients, leaky vascular abnormalities also appear to play a role in VEGF-independent macular oedema (ME).
Management of ME in retinal vein occlusion (RVO) was reviewed by Paolo Lanzetta, Italy. Three drugs - dexamethasone implant, ranibizumab and aflibercept - are now approved for the treatment of ME due to RVO supported by evidence from pivotal trials such as GENEVA, CRUISE and COPERNICUS. Dr Lanzetta noted that early treatment affords better results and recommended use of an as-needed retreatment protocol with monthly follow-up when choosing the dexamethasone implant. The treatment armamentarium in RVO-ME is also continuing to expand with a number of investigational agents in the clinical pipeline.
“The current evidence indicates that intravitreal pharmacotherapy is effective in ameliorating vision function in RVO-ME patients.”
Paolo Lanzetta, Udine, Italy
Discussing the surgical management of resistant cases of vein occlusion, Jose Garcia Arumi, Spain, highlighted vitreoretinal traction and persistent ME resistant to medical treatment as indications for pars planar vitrectomy (PPV). However, the role of PPV in diffuse or non-tractional ME remains controversial. Vitrectomy with internal limiting membrane (ILM) peeling may achieve visual improvements, with effects potentially enduring for years with minimal additional treatments.
Francesco Bandello, Italy considered the question of whether OCTA is essential in RVO. He noted that microvascular changes in RVO are all readily visible with OCTA, which is better than FA and OCT for visualising microvascular changes and cystoid spaces. However, OCTA is unable to view peripheral vascular occlusion due to an insufficiently wide field. Artefacts, such as shadowing of oedema or haemorrhage can also potentially lead to overestimation of ischaemia, and there is inaccuracy of segmentation.

OCTA can detect multiple changes to the vasculature of the retina
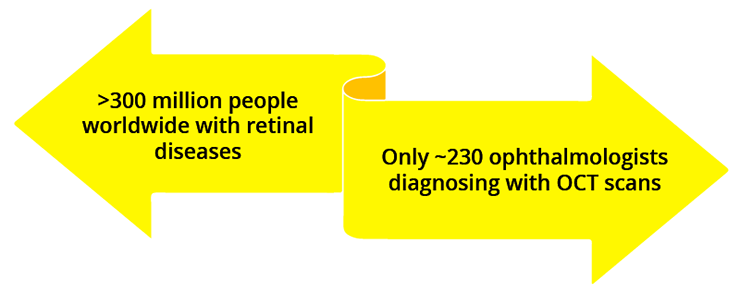
Use of OCT for diagnosis is low on a global scale
Dr Schmidt-Erfurth took delegates on what she described as an ‘AI driven journey into the fluid universe’ in retinal disease. AI is part of an ongoing paradigm shift in retinal diseases being driven by increased availability of therapeutics and the need for timely diagnosis/intervention. In terms of fluid, correlation is dependent on both disease entity and changes over time, with better correlation between central retinal thickness (CRT) and fluid in RVO and DME versus nAMD. The location of the fluid is also important. Dr Schmidt-Erfurth cautioned that CRT is not a universally applicable tool and may be inappropriate to reflect disease activity. AI based segmentation offers fluid quantification with realistic determination of volumes, precise localisation, improved structure/function correlation and guidance for treatment.
Impact of COVID on Retinal Anti-VEGF Outcomes
In an interactive panel discussion session, a group of nine European experts considered the impact of the COVID-19 pandemic on retina care. Recently published data from the UK highlight the stark consequences of lockdown:
- 72% fall in new AMD cases compared with expected across four leading treatment centres
- modelling suggests a delay of 3 months could lead to a >50% relative increase in the number of eyes with vision ≤6/60
- 25% relative drop in the number of eyes with driving vision at 1 year
The panel confirmed that this dramatic fall in patients presenting for both acute/chronic pathologies has been mirrored across most European countries. A substantial reduction was also noted in patients coming to hospital to receive anti-VEGF injections during the pandemic - undoubtedly contributing to vision loss. In the most part, this was attributed to patients’ own anxieties and concerns after attending hospital rather than reductions in actual capacity/care provision per se. Experts also reported an increased incidence of patients with proliferative vitreoretinopathy (PVR) detachment as a direct result of the pandemic.
In terms of strategies for providing clinical care during the COVID-19 crisis, common approaches adopted across European treatment centres included safe spacing, personal protective equipment (PPE), increased gaps between clinic visits, deferral of less urgent cases (vein occlusion and diabetes) and phone calls/information sheets to encourage patient attendance. The panel was particularly impressed with the innovative Israeli approach described by Dr Lowenstein where mobile units were set up capable of delivering anti-VEGF injections in patients’ own homes. Moving forward, experts agreed that valuable time could be saved at each clinic visit by not testing VA routinely.
The impact of the COVID-19 pandemic on clinical trials was also stark, with panel members describing an ~80% decline in patients reporting for trials. This has led to enrollment holds, significant delays in the advancement/approval of new therapies and major issues with missing data (particularly as regards statistical analysis for the primary endpoint).
From a surgical perspective, concerns early on in the pandemic centred on risks to surgeons from the infectious load, which led to the deferral of most laser procedures.
Encouragingly, experts reported that most surgical capacity in Europe is now almost back to normal - albeit with a significant backlog. The majority of centres have adopted an approach of mandatory COVID-19 testing for patients before surgery. However, concern was expressed that a significant second wave could still lead to further operating room closures, with lack of anaesthesiologists highlighted as a significant potential problem. On the future of educational meetings and international congresses, the panel agreed that a mixture of both face-to-face and virtual events was likely to remain the ‘new normal’ moving forward.
“We are now entering a second wave and this is an important challenge which we as ophthalmologists have to face.”
Adnan Tufail, London, UK
ASRS Symposium
Novel gene therapy approaches for inherited retinal diseases were reviewed by Kourous Rezaei, USA, focussing on the IVERIC Bio pipeline. Phase 1/2 trials are scheduled for initiation in 2021 for two potential best-in-class candidates: IC-100 for rhodopsin-mediated autosomal dominant RP and IC-200 for BEST-related retinal diseases. A number of minigene programs are also under evaluation at the research stage including miniCEP290, miniABCA4 and miniUSH2A. As the name suggests, minigenes are engineered to be smaller in size so better able to fit into the preferred AAV vector.
Tarek Hassan, USA and his team carried out a study to investigate predictors of endophthalmitis after intravitreal injection. A total of 98,960 unilateral injections were analysed over a period of 39 consecutive months, from which 40 eyes developed endophthalmitis (0.04% incidence). Results of stepwise multivariate analysis revealed that the only independent predictor for endophthalmitis was the use of viscous topical anaesthetics, with lidocaine gel and tetracaine hypromellose drops increasing the risk by x11 and x4, respectively.

Variables associated with endophthalmitis following intravitreal injection
Dr Tufail discussed the potential of synthetic control arms in clinical trials where statistical methods are used to evaluate the comparative effectiveness of an intervention with external control data. A comparison of bevacizumab to aflibercept using this method suggested the two intravitreal drugs are equivalent for improving VA by 2 and 3 ETDRS lines and for limiting loss of vision to within 3 lines at 24 weeks. By leveraging existing datasets and trials of established retinal disease entities, this synthetic approach has the potential both to accelerate the clinical development process and reduce costs.
New anti-VEGF agents were reviewed by Peter Kaiser, USA. He explained that several new anti-VEGF agents with similar efficacy but enhanced durability are coming down the track including brolucizumab, abicipar pegol, conbercept, KSI-301 and OPT-302. A raft of biosimilars for existing anti-VEGF agents are also on the clinical development horizon. Several sustained release strategies are additionally being pursued including gene therapy and PDS. With all these new agents and approaches to VEGF inhibition, safety remains a paramount consideration, Dr Kaiser cautioned.
“Roughly 1 in 4 ophthalmology trials are single-armed without a comparator, making informed decisions to proceed to further phases of clinical trials difficult.”
Adnan Tufail, London, UK

Comparison of anti-VEGF agents with different mechanisms of action
A talk on the small gauge surgery of myopic foveoschisis (MF) was given by Francesco Boscia, Italy, He explained that observation is the best strategy for most uncomplicated MF but that for complicated cases, PPV with ILM peeling gives favourable anatomic and functional outcomes for different patterns of myopic traction maculopathy. Visual recovery is related to both baseline best corrected visual acuity (BCVA) and inner/outer segment layer recovery. The higher incidence of foveal atrophy in the macular hole group explains the reduced visual recovery despite closure. Overall, evidence suggests that early surgical intervention before the development of macular traction complications may improve visual outcomes, Dr Boscia concluded.
Prof Rizzo presented real-life work undertaken to assess the occurrence of peripheral vitreoschisis-induced vitreous cortex remnants (p-VCR) in primary rhegmatogenous retinal detachment (PPRD) with complete posterior vitreous detachment (PVD) and investigate recurrence risk after PPV. Results showed a significant reduction in re-detachment risk - from 8.1% to 2.6% - when PPV was carried out with VCR check and removal compared to without.
Beyond 2020: New Frontiers in Retina Innovation
Prof Spaide explored the idea of ‘going deep’ in choriocapillaris imaging using a machine learning approach. Machine learning can overcome the segmentation problem of OCT by converting it to a pixel classification problem and is able to generate features based on edge detection, texture etc. With high resolution OCT now facilitating imaging of details not previously seen, Prof Spaide explained that machine learning will be key to extracting vessel information. The resulting data exist in 3 dimensions and can be displayed as such - for example, showing connections to the deep capillary plexus.
Sirinivas Sadda, USA summarised key areas of advancement in OCT imaging expected for the future (Figure). Ultimately, these developments may lead to the advent of an OTC Diagnostics Centre, where the functions of many different devices and people are distilled down into one low-cost device.
“We are in the midst of a golden era of retinal OCT imaging.”
Sirinivas Sadda, Los Angeles, USA

Advances in OCT imaging
Gemma Cheung, Singapore, discussed future advances in imaging technologies for myopia which will enable clinicians to evaluate myopia pathogenesis and pathology in more tissue layers, 3-dimensionally and dynamically. Dr Cheung proposed that these advanced imaging data could be used to complement clinical trial data, longitudinal follow-up and serum/ocular biomarkers to further our understanding of the development and progression of myopia and its complications.
TELEOPHTHALMOLOGY
- Describes remote eye care carried out using audiovisual telecommunication technology
- Advances in the field driven by better cameras able to incorporate other diagnostic tests and AI
- Increasing retinal diagnostics and screening will take place outside the doctor’s office in homes and community setting in the future
AUGMENTED REALITY (AR)
- Different from virtual reality because it enhances rather than replaces the real world, with digital elements overlaid over real-world surroundings
- Oculenz, the first AR device developed for low vision, anticipated to be available mid 2021
- Oculenz uses pixel mapping around the blind spot in AMD and incorporates the capacity for both visual field testing and in-home monitoring
ARTIFICIAL INTELLIGENCE (AI)
- ‘Fourth industrial revolution’
- AI able to see what humans cannot in both fundus and OCT imaging
- Deep learning proven superior to retina experts in predicting progression from dry to wet AMD
- Five ‘rights’ for a successful AI project in ophthalmology: the right questions, right data, right partner, right concepts and right enabler.
EURETINA Guidelines for the Management of Retinal Disease: The Next Steps
Ursula Schmidt-Erfurth, Austria explained how AI has afforded new insights into nAMD. Fluid volume can now be precisely identified, localised and measured by deep learning and automated algorithms are available such as the Vienna fluid monitor. AI evidence has revealed that, although central subfield thickness (CSFT)/CRT does not correlate with fluid in nAMD, fluid matters in all compartments. Intraretinal fluid (IRF) has a negative impact on BCVA while subretinal fluid (SFR) is associated with a better prognosis, but benefits from retreatment.
“Objective and accurate fluid quantification is the future for optimised management of AMD, which is a leading cause of blindness”
Ursula Schmidt-Erfurth, Vienna, Austria
Shoba Sivaprasad, UK reviewed diagnostic and therapeutic guidance on DR severity. The current rating of DR severity relies on 7-field colour fundus photographs. However, this is likely to change in the future based on multimodal imaging. Hyperglycaemia, hypertension and hyperlipidaemia remain the key risk factors for DR development and Dr Sivaprasad stressed the importance of maintaining HbA1c below 7.6% in T1DM. PRP is the current standard of care for proliferative diabetic retinopathy (PDR) and should be carried out adequately, with patients followed-up for at least 5 years. Anti-VEGF (vascular endothelial growth factor) also represents a non-destructive disease-modifying treatment for PDR. However, this therapeutic approach does not improve capillary non-perfusion (CNP) so new treatments will still be needed moving forward.
OCT has arrived at a consensus definition for lamella macular holes (LMH) with three clinical entities defined: LMH, epiretinal membrane (ERM) foveoschisis and macular pseudohole (MPH) - each of which can be identified by mandatory criteria and optional anatomical features. Ramin Tadayoni, France discussed the surgery of these (pseudo)holes and standards in macular surgery. For LMH, he explained that multiple papers have now been published showing the success of surgical techniques (e.g. a double-inverted flap technique) in improving vision. However, randomised, controlled trials are still needed to confirm the benefits of this approach. For ERM foveoschisis and ERM with macular pseudohole, the standard treatment with membrane peel is recommended.
Anat Loewenstein, Israel reviewed increasing options in heads-up surgery, focusing on two novel technologies for intraoperative vitreo-retinal imaging: the Heads-Up 3D Display and head wearable devices. The Heads-Up 3D system comprises dynamic range cameras which capture the image from the patient’s eye and display it on a large viewing monitor - thereby offering important teaching and training opportunities. Head wearable devices contain no microscopes and are completely controlled by head gestures. Devices can accommodate multiple virtual displays which are customised for the surgeon’s needs and provide real-time access to data with no lag or perceived latency. Dr Loewenstein confirmed that these new surgical tools have multiple applications and have now been validated in 120 successful surgeries carried out in the US and Israel including vitrectomy, retinal detachment and removal of lens fragments.
“The ability to transmit this 3D view to monitors and screens outside the operating room is a very valuable tool for live-surgery meetings.”
Anat Loewenstein, Tel Aviv, Israel
The European response to the myopia pandemic was examined by Caroline Klaver, the Netherlands. Dr Klaver explained that high myopia, which carries the heaviest visual burden (Figure), is predicted by early age of onset and driven by environment over genetics. According to a recent International Myopia Institute report, axial length should be the target in myopia control and three effective interventions have been identified: multifocal contact lenses, Ortho-K lenses and atropine. In a 3-year Dutch study involving 124 children, atropine 0.5% reduced myopia progression by 75%. Safety issues such as photophobia and reading difficulties were successfully resolved with multifocal photochromatic glasses.

High levels of myopia are associated with risk of visual comorbidities
“High dose atropine is a good response to the European myopia pandemic.”
Caroline Klaver, Rotterdam, the Netherlands.
Closing Remarks
Looking ahead to next year, the 21st congress of EURETINA is scheduled to take place in Barcelona, Spain between the 9th and 12th September 2021. However, Prof Holz explained that, as the largest society of retina specialists in Europe, the scope of EURETINA extends far beyond the congress itself and that a strategic roadmap stretching to 2025 has now been created, outlining the society’s plans and priorities over the next 5 years.
©Springer Healthcare 2020. This content has been independently selected and developed by Springer Healthcare and licensed by Roche for Medically. The topics covered are based on therapeutic areas specified by Roche. This content is not intended for use by healthcare professionals in the UK, US or Australia. Inclusion or exclusion of any product does not imply its use is either advocated or rejected. Use of trade names is for product identification only and does not imply endorsement. Opinions expressed do not reflect the views of Springer Healthcare. Springer Healthcare assumes no responsibility for any injury or damage to persons or property arising out of, or related to, any use of the material or to any errors or omissions. Please consult the latest prescribing information from the manufacturer for any products mentioned in this material.