Burden of disease
Global burden of Chronic Liver Disease
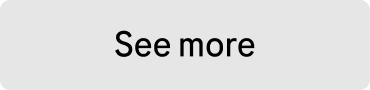
Globally, approximately one in five people suffer from chronic liver disease,1 despite 90% of cases being preventable.2
CLD was related to over 1.3 million deaths in 2017, mainly among men, and associated with an increasing incidence of obesity and alcohol consumption.1 The absolute number of CLD cases is estimated at 1.5 billion worldwide, with the most common causes of disease including non-alcoholic fatty liver disease (NAFLD) (59%), infection with viral Hepatitis (HBV or HCV) (38%), and alcohol-related liver disease (ALD) (2%).1
- Challenging diagnosis: Signs and symptoms of CLD can be nonspecific, such as fatigue, anorexia, weight loss, or depend upon the complication that the patient has developed.4 It is estimated that <2% of potential CLD patients have been diagnosed.3 The three ‘classical’ complications are associated with the progression of fibrosis to liver cirrhosis and comprise portal hypertension (esophageal varices, ascites), hepatocellular insufficiency (e.g., jaundice, hepatic encephalopathy), and hepatocellular carcinoma.4
- Social stigma and poor prognosis: Perceived stigma is common among CLD patients, regardless of disease aetiology. CLD stigma is associated with impaired quality of life5,6 and contributes to a delay or failure in seeking help, and risks delaying the ‘cascade of care’ (screening, referral, treatment) resulting in negative health outcomes.5,7,8
- Need for early screening: Identifying liver disease in ‘healthy’ at-risk populations is challenging within health care systems already struggling to provide high standards of care to patients with established disease. Historically, the primary method of identifying patients with CLD has been liver function tests (LFTs). However, most people with abnormal LFTs do not have liver disease.2 CLD is usually diagnosed late in the disease process. Earlier diagnosis would permit interventions (e.g., alcohol interventions, antiviral therapies, weight loss) before the onset of irreversible disease or progression to liver cancer.2
- Preventing progression from CLD to HCC: The epidemiology of CLD is shifting from viral etiologies to reflect the rising prevalence of metabolic syndrome and alcohol misuse.6 A key goal of disease management is to disrupt the CLD continuum and prevent progression to liver cancer.6 Patients with CLD who are at risk of developing liver cancer require surveillance and regular monitoring,4 with a broadening of prevention and treatment strategies.6
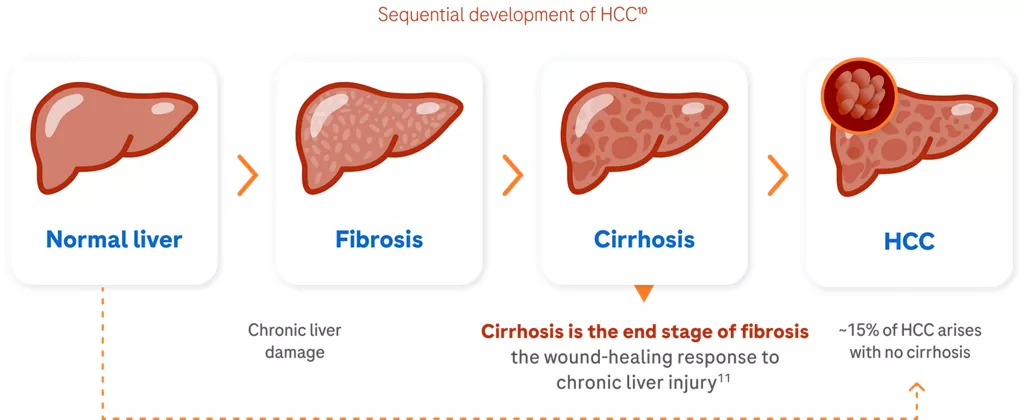
Undiagnosed CLD can progress to Liver Cancer
People with undiagnosed CLD can silently progress to liver cirrhosis, placing them at high risk of developing hepatocellular carcinoma (HCC); up to 10% of people with liver cirrhosis may progress to HCC.2,9 Cirrhosis and liver cancer account for 3.5% of all deaths worldwide.6
Global burden of HCC
Today, millions are progressing silently through the CLD continuum towards developing liver cancer.
Liver cancer is the sixth most common cancer worldwide12 and is a complex, deadly disease.9 Potential curative options exist for patients in early settings;13 however, early HCC remains an area of high unmet need.9,14

Third leading cause of cancer death: HCC comprises approximately 90% of all liver cancers and is the third leading cause of cancer death worldwide.9 In 2020, there were an estimated 900,000 new liver cancer cases (75% increase from 1990) and 830,000 cancer-related deaths worldwide.12 The most significant increases in liver cancer-related mortality were in North America, Europe, and Australia.6

Rising Global incidence: Despite advances in treatment options,13 the global incidence and mortality of HCC continue to rise6 and constitute a worldwide health challenge.9 By 2025, over 1 million patients per year will receive an HCC diagnosis compared with 840,000 in 2018 – a relative increase of almost 20%.9,12 Global deaths from liver cancer are predicted to increase by more than 50% by 2040.12
References
1. Cheemerla S. and Balakrishnan M. Clin Liver Dis (Hoboken) 2021;17:365–70.
2. Macpherson I, et al. Frontline Gastroenterol 2022;13:367–73.
3. American Liver Foundation. How Many People Have Liver Disease?Available at: https://liverfoundation.org/about-your-liver/facts-about-liver-disease/how-many-people-have-liver-disease/ [accessed August 2023].
4. Sharma A, et al. Chronic Liver Disease. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554597/
5. Carol M, et al. PLoS ONE 2022;17(4):e0265153.
6. Moon AM, et al. Clin Gastroenterol Hepatol 2020;18:2650–66.
7. Schomerus G, et al. J Hepatol 2022;77:516–24.
8. Vaughn-Sandler V, et al. Dig Dis Sci 2014;59(3):681–6.
9. Llovet JM, et al. Nat Rev Dis Primers. 2021;7(1):6.
10. Marquardt JU, et al. Nat Rev Cancer 2015;15(11):653–67.
11. Pinter M, et al. ESMO Open 2016;1:e000042.
12. Rumgay H, et al. J Hepatol 2022;77:1598–1606.
13. Zhu X-D, et al. Genes & Diseases 2020;7:359–69.
14. Minami Y, et al. Hepatobiliary Surg Nutr. 2019;8(4):414–6.
15. Vogel A, et al. Ann Oncol 2021;32(6):801–5.
16. Reig M, et al. J Hepatol 2022;76:681–93.
17. Ginès P, et al. Hepatology 2022;75(1):219–22.