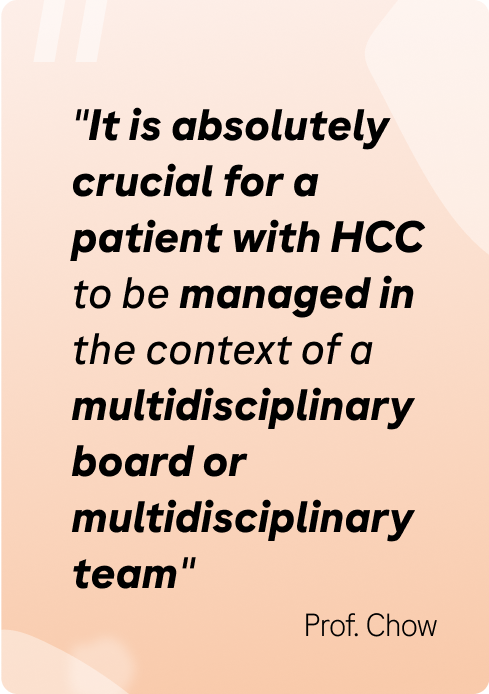
Multidisciplinary Team approach to HCC care
Utilization of a multidisciplinary team (MDT) in HCC
A holistic, multidisciplinary approach significantly improves outcomes in patients with HCC through early diagnosis and intervention
The MDT is an alliance of medical and healthcare professionals dedicated to managing a specific tumor disease, with a focus on evidence-based clinical decisions and coordination of care delivery across all stages of the management and treatment.1 As the clinical features of hepatocellular carcinoma (HCC) are often subtle and nonspecific, management by MDT permits care providers with different roles, expertise and functions to provide optimum patient care.1,2
The core members of an HCC MDT include liver surgeons, hepatologists/gastroenterologists, oncologists, interventional radiologists, pathologists, and primary care physicians, with additional consultative experts included based on the individual needs of the patient.2,3
Value of an MDT in HCC
A multidisciplinary holistic approach to HCC care improves diagnosis rates, referral pathways, access to treatment, and ultimately, patient survival4
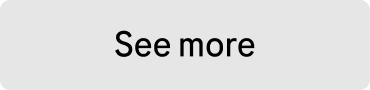
MDTs reduce the waiting time from referral to treatment and accelerate the diagnostic process of HCC, mainly due to a reduction in time from referral to the first visit and time from first visit to MDT treatment decision.5
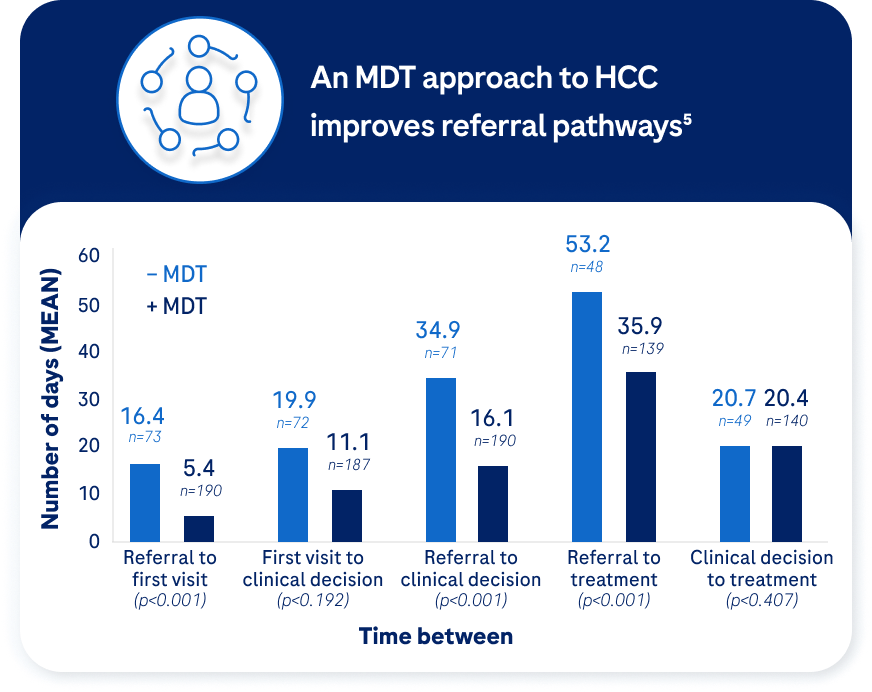
Limited access to an MDT may hinder time to HCC diagnosis, with patients presenting later at a more advanced disease stage.4 Establishment of an MDT HCC clinic is associated with improved diagnoses at an earlier disease stage, with reduced time to diagnosis and treatment potentially resulting from having all providers (e.g., surgeons, interventional radiologists, and medical oncologists) present in the clinic setting – eliminating untimely delays from scheduling multiple physician visits on different days in varying clinic settings.4
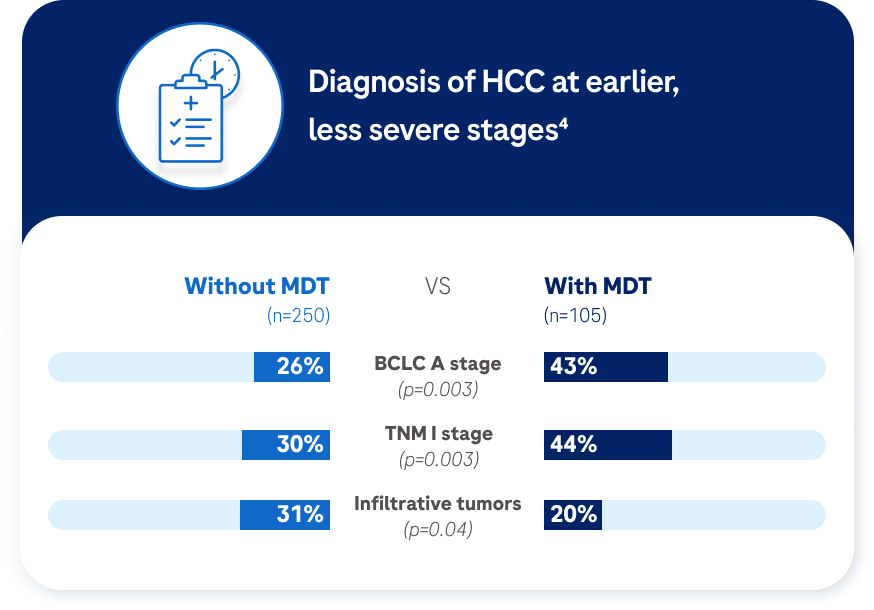
When an MDT approach is applied, HCC patients have a significantly increased rate of receiving an appropriate, individualised treatment plan with associated increases in improved survival.6
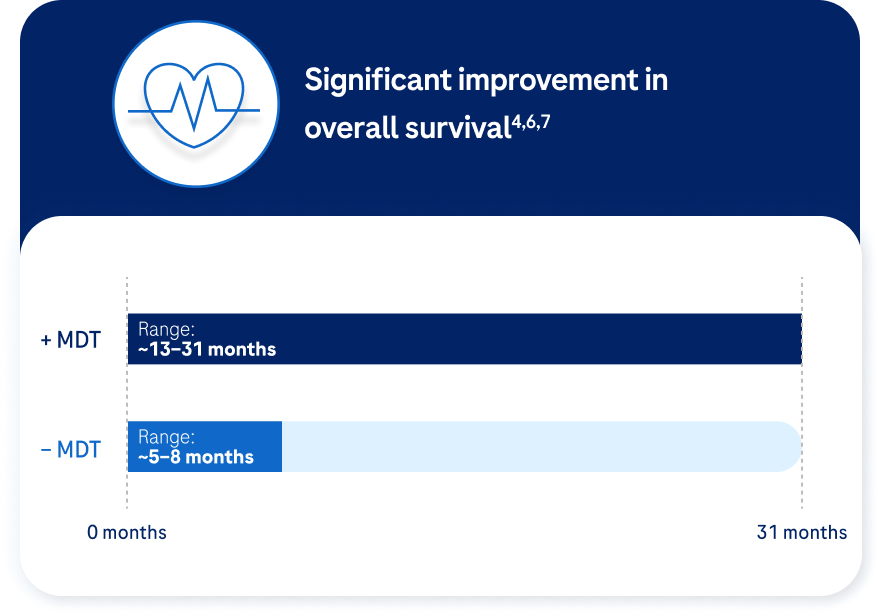
An MDT holistic approach improves diagnosis rates, referral pathways, and access to treatment. Ultimately, HCC MDTs are associated with improved overall survival, independent of tumor stage.4
Barriers to establishing an MDT in HCC
Patients perceive the MDT setting as superior to the more traditional care ‘serial’ clinic model.8 However, there can be significant barriers to accessing MDT-based care.1,9
There are several obstacles to creating and managing a successful HCC MDT. A highly complex and variable decision-making process4,10 can be further compounded by local policies and funding restrictions,1,9 inequalities in patient access,9 and weak communication and collaboration across the MDT team.3
HCC is a complex disease: As the complexity and cost of HCC management increases, the need to collect and provide evidence on the cost benefits of an MDT becomes more important for obtaining buy-in from hospital administrations.9

Healthcare policies: Despite clinical evidence supporting the functionality of MDTs, healthcare policies to support MDT management of HCC are often lacking due to limited resources, team capacities, and cost issues.1

Funding: Lack of funding often means that the healthcare team must donate the extra time and effort to make the MDT a reality – hospitals may need to allocate funds to reimburse the MDT service.9
Patient access: Equal access to speciality care remains a challenge in areas where communications among providers and streamlined processes are lacking. In under-served populations, access to speciality care remains a particular challenge.9

Integrated working: HCC management requires the involvement of multiple specialists to provide individualised treatment strategies. These specialists must find ways to coordinate and communicate treatment recommendations and collaborate on patient management within the confines of local procedures and resources.9
Overcoming MDT barriers

Administration: Administrative support is key to the success of an MDT programme, and a nurse specialist in HCC or a hepatobiliary oncology is critical for administering and coordinating the programme. In addition, an acknowledged leader of the consensus group is important for both clinical decisions, quality control, as well as providing direct outreach to the local community.9

Telemedicine: Many MDTs utilise telemedicine or teleconferencing to permit virtual participation of other non-local providers using real-time videoconferencing to share knowledge. Such technology is especially relevant for centers that lack full resources or necessary local specialists.9
Different MDT models: Depending on local needs and available resources, different models of MDT care may be considered, ranging from a multidisciplinary tumor board to a fluid referral system between specialties to a co-located clinic.3

Regular meetings: Regular MDT meetings provide many benefits, such as enabling input from all MDT members, providing time to develop comprehensive treatment plans, minimising communication errors and delays in treatment, and increasing member awareness of new research in related fields.9
References
1. Sinn DH, et al. PLoS One 2019;14:e0210730.
2. Siddique O, et al. Journal of Multidisciplinary Healthcare 2017;10:95–100.
3. Byrd K, et al. Semin Liver Dis 2021;41:1–8.
4. Yopp AC, et al. Ann Surg Oncol 2014;21(4):1287–95.
5. Villadsen GE, et al. J Gastrointestin Liver Dis 2019;28(1): 83–8.
6. Duininck G, et al. J Surg Oncol 2019;120(8):1365–70.
7. Agarwal PD, et al. J Clin Gastroenterol 2017;51(9):845–9.
8. Soares KC, et al. Ann Surg Oncol 2014; 21:1059–61.
9. Naugler WE, et al. Clin Gastroenterol Hepatol 2015;13:827–835.
10. Reig M, et al. Journal of Hepatology 2022;76:681–93.