Welcome to ESMO 2022
-
The Annual Meeting of the European Society of Medical Oncology (ESMO) was a hybrid meeting, with delegates attending in person for the first time since before the pandemic. ESMO President Solange Peters noted that this made the meeting “feel like a huge success before it has even begun” as the oncology community were able to meet, network and disseminate data in-person in Paris, France. She underlined that, for ESMO, there was never going to be a return to “normal” but was instead progressing forward due to the proactivity that the community has demonstrated in reinventing itself to meet the challenges of our era.
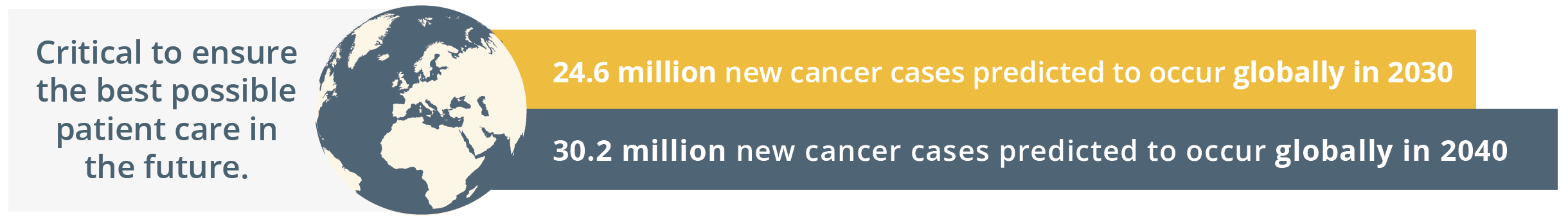
New cancer cases predicted globally by 2030 and 2040
Globally, the ESMO community is already taking action by going the extra mile to comfort patients, to grow as professionals by keeping their knowledge up-to-date, and by raising awareness for cancer prevention. The ESMO community is driven by a shared determination to work towards the best possible outcomes for patients with an inspiring tagline of, ‘Together we can. Together we care.’
Solange Peters then summarised the importance of healthcare sustainability and how our healthcare systems rely on finite resources. She emphasised that a key responsibility of the oncology community should be safeguarding patients’ ability to access high-quality care. ESMO should continue to contribute to the overall sustainability of the healthcare system by nurturing the professional development of oncologists and offering continued support in their day-to-day clinical practice. ESMO’s support and resources should therefore reach every oncology professional.
“As important as doctors’ knowledge and skill is their physical and mental ability to give the best of themselves to patients each day.”
- Solange Peters, ESMO President
Solange Peters then introduced the ESMO 2022 Scientific Co-Chairs, Fabrice André and Charles Swanton. Charles Swanton gave an overview of the impressive proportion of delegates attending ESMO 2022 both in-person and online. He then stated that the purpose of ESMO 2022 is not only a “celebration of getting us all back together”, but also a collaboration between diverse oncology professionals who spend their lives aiming to improving the survival of their patients. ESMO 2022 will focus on “better understanding the disease and treating patients better – from bench to bedside”, which is a matter of time, collaboration, patience and long-term investment. Fabrice André added that current challenges in oncology will be integrated within the ESMO Congress 2022 programme such as early cancer detection and prevention, molecular medicine, and the impact of new drugs assessed in underrepresented patients such as anti-programmed cell death protein-1 (PD1) in the elderly population.
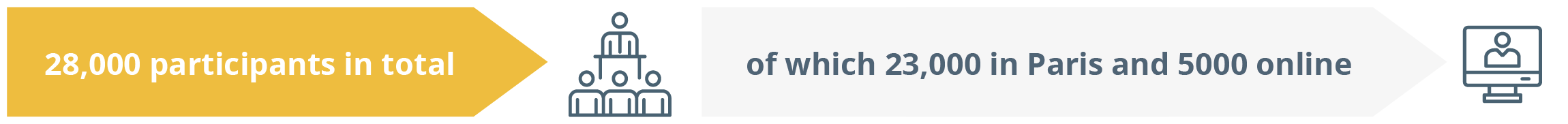
Total participants online and in person
COVID-19: Patient Advocacy
The Time to Act Campaign
Mark Lawler, Belfast, Ireland, gave a startling statement that “People are starting to fear a COVID-19 diagnosis more than a cancer diagnosis,” and that, based on data from Hospital Trusts across the UK, 7 out of 10 people with suspicion of cancer were not going to their GP and 4 out of 10 patients with cancer were not able to access their chemotherapy. Disruption was seen across the entire cancer pathway from diagnosis to treatment. A recent analysis found that 500,000 endoscopies were delayed due to the COVID-19 pandemic, which is a crucial diagnostic procedure for many gastrointestinal cancers. Real-time data were also analysed from approximately 4-million citizens to inform a model that predicted 7165 to 17,910 excess deaths, suggesting that the COVID-19 pandemic resulted in excess mortality.
In light of the impact of the COVID-19 pandemic, the Board of the European Cancer Organisation and the World Health Organisation Europe developed a 7-point plan to mitigate the impact of COVID-19.

7-point plan to mitigate the impact of COVID-19
A “time to act” campaign at the European level was also underpinned with evidence-based intelligence to put cancer at the top of the Recovery Agenda. He said it was worrying how we are in a race against time to find missing cancer diagnosis as 100 million cancer screening tests were not performed in Europe and 1 million cancer patients could be undiagnosed due to the presentational backlog.
“We demand – not ask – that cancer must be put at the top of the European Health Agenda.”
- Mark Lawler, Belfast, Ireland
The message is stark – the time to act is now. A new award-winning landmark tool, the “Time to Act Data Navigator”, has been developed with initial surveillance data from 17 European countries presented in a patient-friendly manner. The powerful tagline for the Time to Act campaign is, “Don’t let COVID-19 stop you from tackling cancer.”
Impact of COVID-19 on surgery
Françoise Rimareix, Villejuif, France, bolstered Mark Lawler’s point that there were significant delays due to the COVID-19 pandemic, particularly in surgery. She discussed a recent analysis of data from 466 hospitals across 61 countries (N=20,006 with 15 cancer types) that found 10% of patients did not receive surgery after a median follow-up of 23 weeks. She emphasised that cancer surgery systems worldwide were fragile due to the lockdowns, with an increase in non-operate rate due to the full lockdowns.
“We can say, unfortunately, that the impact on cancer treatment is a collateral damage of the pandemic.”
- Françoise Rimareix, Villejuif, France
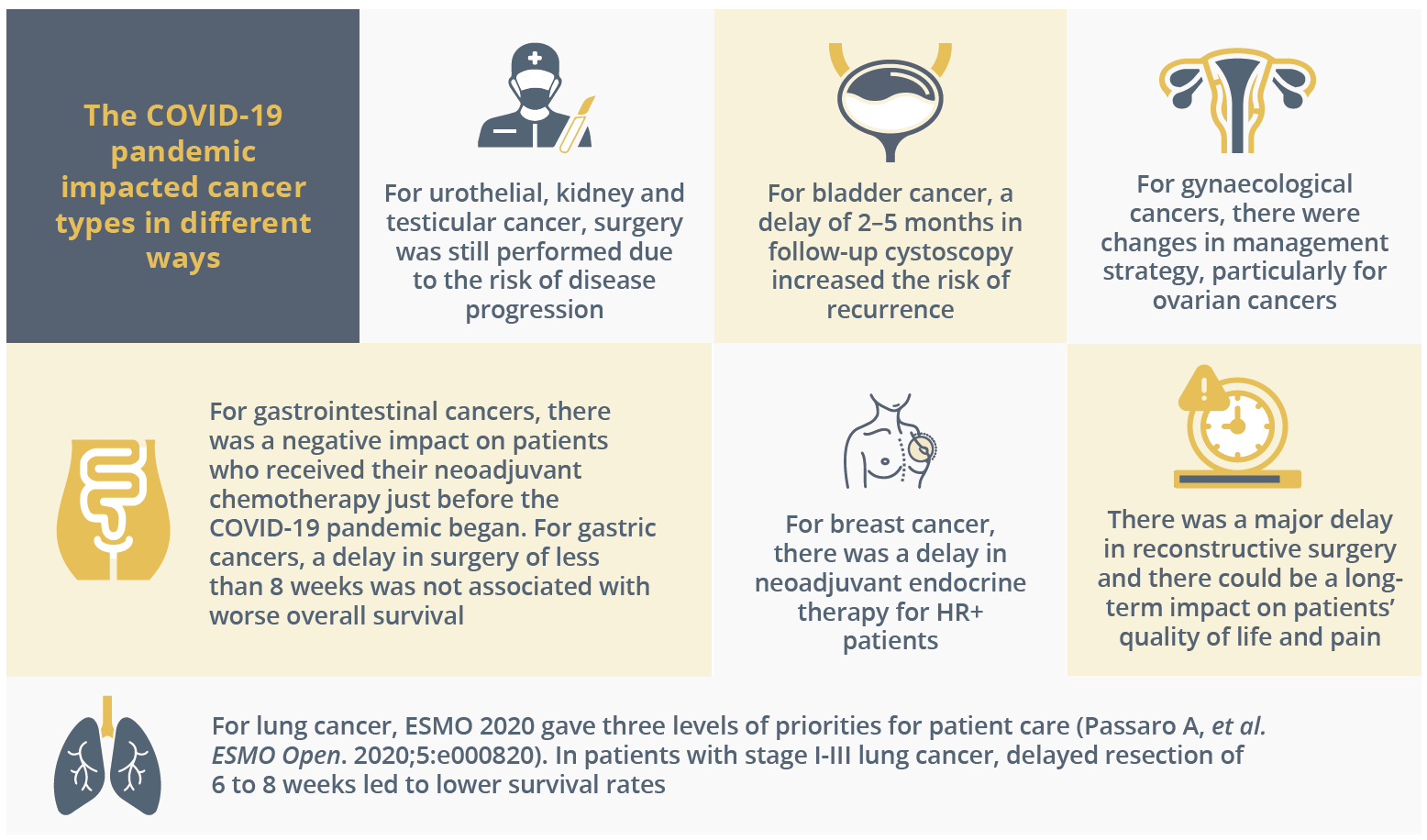
How the COVID-19 pandemic impacted patient care for GI, breast, bladder, lung, gynaecological and GU cancers
There needs to be a modification of healthcare systems to avoid the cumulative delay in surgery for patients with cancer. As the effects of the delays in surgery will take years to be fully understood and could become challenging to manage, prioritisation of oncologic surgery and long-term investment in surgical capacity is required. The impact on surgery is assumed to be worse in developing countries, but data are required to confirm this.
The impact of the COVID-19 pandemic on telemedicine
The COVID-19 pandemic resulted in a major shift in the use of telehealth services. Remote consultations took priority when there was a dramatic decrease in all follow-up appointments in April 2020 compared with April 2019. Patients’ and oncologists’ perspectives on telemedicine implementation during the COVID-19 pandemic were assessed with quantitative surveys in May and June 2020, particularly whether virtual solutions could be considered a substitute for in-person consultations and if it could enhance physician-patient communication. In May and June 2020, 101 and 468 oncologists and patients with cancer responded, respectively; 61% of oncologists would want to utilise video consultations, whereas only 15% of patients preferred this option. A follow-up survey was conducted in August 2022 and received responses from 202 patients; 42% of patients said they would like to take advantage of the option of a video consultation. Important benefits of telemedicine for patients were quicker access to a doctor’s advice and comfort. For oncologists, important benefits were a reduction in cost due to transportation and sparing the patient’s time.
Ivica Ratosa, Ljubljana, Slovenia, suggested factors that may have impacted physician-patient communication over the past two and a half years:
- The COVID-19 pandemic resulted in a rapidly changing healthcare environment, disrupting communication among physicians, patients and their families
- Clinical processes could have been insufficient to adequately support the use of telemedicine
- Physicians’ limited clinic time to talk to patients
- Physicians’ limited time and attention to learn new skills
She also highlighted major obstacles in the field of telehealth and oncology:
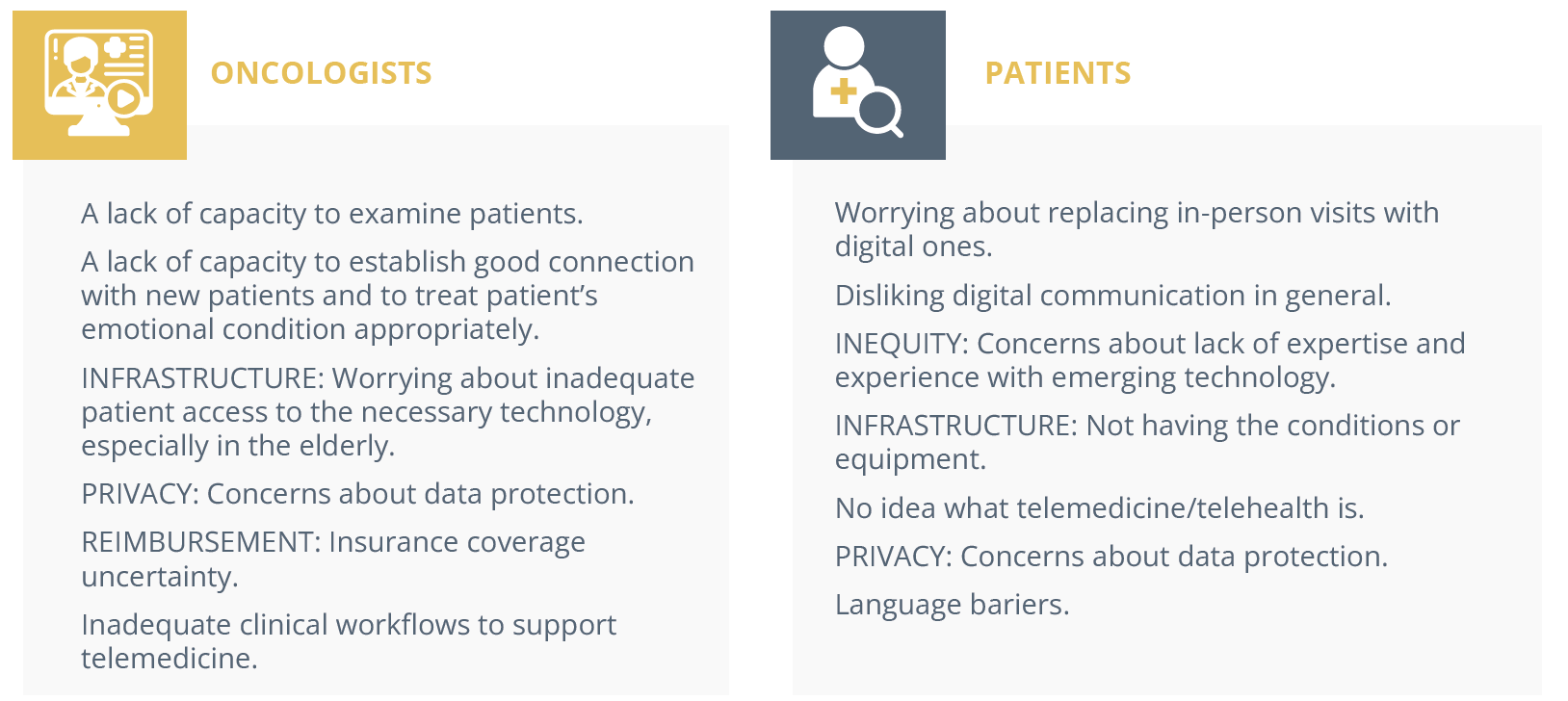
Obstacles preventing uptake of telehealth practices for oncologists and patients
In conclusion, she considered telemedicine a cost-effective alternative way to deliver oncology care. However, telemedicine is unlikely to replace in-person visits in oncology, but can complement patient care overall.
Closing Remarks
Following a successful in-person meeting this year with ~23,000 attendees, ESMO 2023 will continue to disseminate the latest cutting-edge data and provide a unique networking opportunity for oncology professionals in-person in Madrid, Spain, from 20–24 October 2023. Save the date for what will be an equally engaging and successful meeting in 2023.