
The 2021 Annual Congress of the American Thoracic Society (ATS) was held between May 14th and 19th and showcased the latest advances and breakthrough discoveries that will reshape the future of respiratory science, patient care and global respiratory health. A robust scientific, educational and networking programme was delivered via the virtual ATS platform, which included clinical and scientific sessions, keynote series, postgraduate courses and meet the expert sessions.
Juan Celedón, ATS President
ATS 2021 got underway with the opening ceremony and an address by current President Juan Celedón, who highlighted the extreme challenges of the past year which ATS has addressed with advocacy and a renewed focus on its over-arching mission to advance research and careers, clinical care and public health. Incoming President-Elect Lynn Schnapp then outlined key priorities and opportunities for the year ahead which include infrastructure upgrades, the leveraging of new learning methods and technologies and an increased focus on collaboration and knowledge-sharing.
“This past year, a once-in-a-century catastrophe has revealed the character and commitment of our ATS members who confronted the COVID-19 pandemic with selfless devotion to prevent further suffering and help those afflicted.”
ATS President, Juan Celedón
INTERSTITIAL LUNG DISEASES (ILD)
Genes, Environment and Treatment: Characterising Risk in ILD
Research based on the Coronary Artery Risk Development in Young Adults (CARDIA) patient cohort has revealed that novel imaging markers of lung injury and inflammation are associated with future interstitial changes in middle-aged adults. Gabrielle Liu, Chicago, USA, described computerised tomography (CT) lung injury as a key imaging feature associated with future interstitial features which represents a distinct phenotype of impaired respiratory health. Systemic inflammation may be associated with the transition from CT lung inflammation to interstitial features.
Samuel Ash, Boston, USA, explained that multiple protein biomarkers, including angiopoietin 2 and matrix metalloproteinase 7, were found to be associated with interstitial features and their progression in smokers in a study using cohorts from the COPDGene Study and the Pittsburgh Lung Screening Study (PLuSS). It may therefore be possible to predict patients’ risk of progression using a combination of clinical and peripheral protein biomarker-based features.
Analysis of data from 283 patients in the Idiopathic Pulmonary Fibrosis-PRospective Outcomes (IPF-PRO) Registry has identified several circulating microRNAs associated with clinically relevant outcomes in patients with IPF, which may warrant future study as candidate biomarkers, said Tracy Luckhardt, Birmingham, USA. These include miR-128-3p which showed a non-linear relationship with respiratory death.
Bina Choi, Boston, USA, highlighted risk features associated with the progression of interstitial features and outcomes in ever-smokers from the COPDGene (N=6409) and PLuSS cohorts (N=639). Several factors were found to be independently associated with the longitudinal progression of interstitial features, while advanced age, current smoking status and MUC5B minor allele copy number were identified as key demographic and genetic risks for progression.
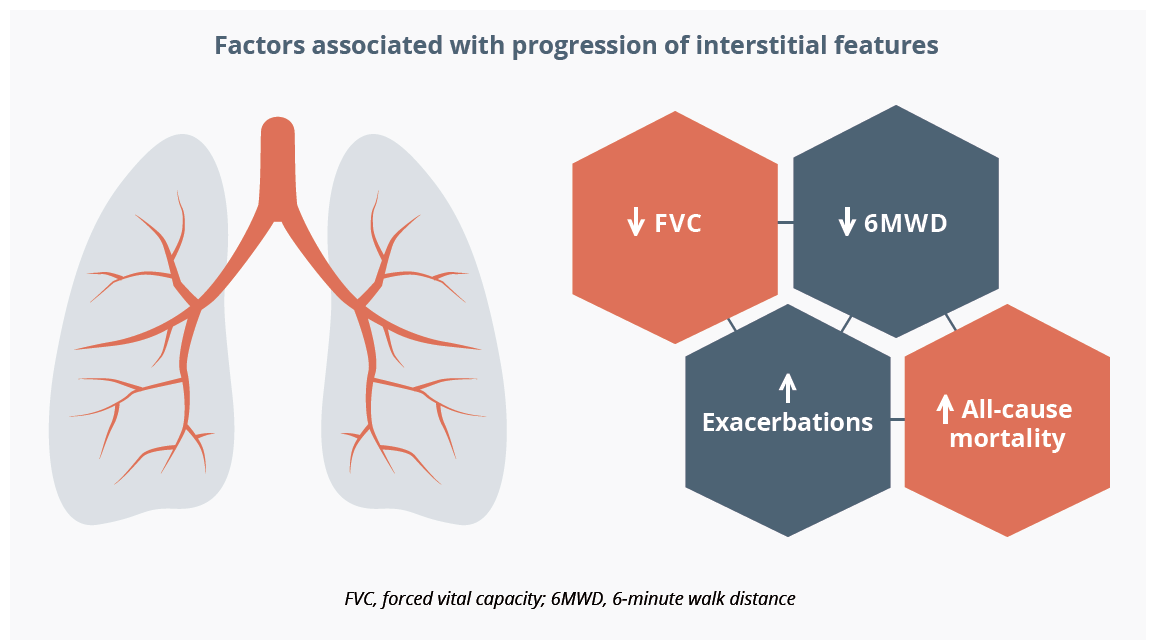
Several factors have been found to be independently associated with longitudinal progression of interstitial features
The project undertaken by Na’ama Avitzur, Calgary, Canada, aimed to characterise the link between environmental health and clinical outcomes using patients with IPF retrospectively identified from the ILD program database at UCSF. Greater relative disadvantage - namely higher environmental exposure to the pollution burden and enhanced social vulnerability - was found to be associated with lower baseline lung function and lower antifibrotic use.
Results from a longitudinal cohort study examining the impact of rurality on 843 patients with IPF referred to a quaternary care centre were discussed by Alison DeDent, San Francisco, USA. Rural individuals were shown to present both with worse baseline pulmonary function and a trend towards increased mortality in their first year of follow-up.

“These findings suggest that rural populations are experiencing delays in their diagnosis of IPF.”
Alison DeDent, San Francisco, USA
Research presented by Deborah Assayang, Montreal, Canada, explored the impact of gender on treatment among 2292 patients with ILD enrolled in a large Canadian prospective cohort. Male gender was found to be significantly associated with earlier treatment initiation across all diagnoses, including IPF. Dr Assayang suggested that possible reasons for this could include the perception of a more favourable prognosis in female patients and their later referral to ILD clinics.
Stacey Lok, Saskatchewan, Canada, showcased findings from a retrospective, multicentre, observational cohort study (N=1157) which probed potential malignancy risks associated with myophenolate mofetil (MMF) and azathioprine (AZA) in patients with fibrotic ILD. Overall malignancy rates were found to be low in patients with connective tissue disease-associated (CTD)-ILD or chronic hypersensitivity pneumonitis (HP) treated with MMF or AZA, and no increased malignancy risk was identified with MMF exposure.
Conundrums and Controversies in ILD Diagnosis and Management
In an interactive pro/con debate session, Marlies Wijsenbeek, Rotterdam, the Netherlands, and Ganesh Raghu, Seattle, USA, deliberated whether or not IPF constitutes a distinct clinical entity. Dr Wijsenbeek argued that classifying IPF has facilitated important clinical progress, and that merging IPF with other non-fibrosing ILDs would only create problems, not solve them. There is also insufficient evidence to support stratifying patients with IPF into different subgroups by disease behaviour or response to therapy, she added. Dr Raghu countered with the suggestion that IPF is a ‘myth’ and a term that was ‘made-up back in the days of ignorance.’ We still talk about IPF and usual interstitial pneumonia (UIP) - the pattern of UIP with honeycomb cysts being an essential component of IPF diagnosis - as if it is an entity of unknown cause, he noted. When in reality our evolved knowledge indicates that UIP is a non-specific pattern and a late manifestation of several heterogenous ILDs including non-specific interstitial pneumonia (NSIP), CTD, HP and occupational lung diseases.
“I submit to you in 2021 that IPF is not a primary entity of unknown cause but simply represents a delayed diagnosis of irreversible pulmonary fibrosis of multiple causes.”
Ganesh Raghu, Seattle, USA
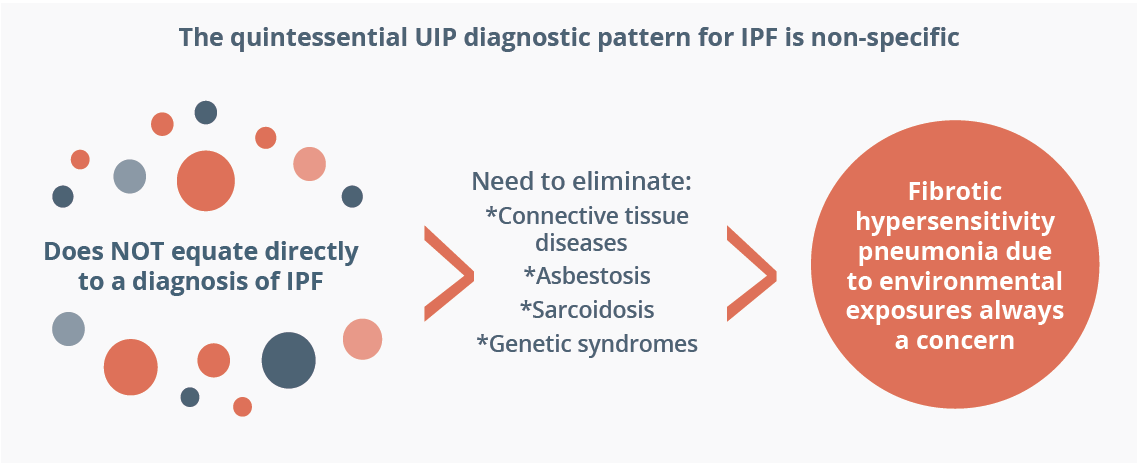
UIP is considered to have a non-specific pattern and does not equate directly to a diagnosis of IPF
Manuela Funke, Bern, Switzerland, and Justin Oldham, Davis, USA, debated whether a genomic classifier from transbronchial lung biopsy specimens is useful in UIP diagnosis. Dr Funke argued that a genomic classifier can support early and accurate diagnosis, improve both the confidence and quality of diagnosis and facilitate differentiation of IPF/UIP from other ILDs. Dr Oldham proposed that the real question should be whether this molecular diagnostic tool can be used to predict a PF-ILD phenotype, irrespective of confidence in the corresponding clinical diagnosis.

The average lung function decline in patients with IPF globally
On the role of transbronchial cryobiopsy in the histopathological diagnosis of fibrotic ILDs, Sonye Danoff, Baltimore, USA insisted that, in well-trained hands, the histopathological yield is excellent, can add substantively to diagnostic certainty and boasts a slightly superior risk profile to surgical lung biopsy (SLB). Lauren Troy, Sydney, Australia disagreed, describing tranbronchial cryobiopsy as ‘too risky, unreliable and frankly unnecessary’. She labelled it as less accurate and less high yielding than SLB and highlighted bleeding as a key safety risk.

“Is it necessary to biopsy at all? ... Increasing evidence for the use of antifibrotics in progressive pulmonary fibrosis and other ILDs really supports a lumping versus splitting approach.”
Lauren Troy, Sydney, Australia
Fernando Martinez, New York, USA, argued in favour of the treatment of non-IPF progressive pulmonary fibrosis (PF) as a single phenotype. He explained that progressive disease is seen in a subset of patients with non-IPF fibrosing lung disease and biological overlap with IPF is significant. Antifibrotic therapy also appears to be effective in this patient population, further justifying treatment. Athol Wells, London, UK, rebutted with the assertion that lumping and splitting of individual ILD disorders are equally deleterious and that a balance is required. Rather than treating as a single-phenotype, non-IPF progressive PF must be managed on a case-by-case basis taking into account key factors such as disease severity and progression, he insisted.
Childhood Interstitial Lung Disease
Jennifer Wamback, St Louis, USA, gave an update on clinical and research progress in childhood ILD (chILD), which comprises 200 rare heterogenous respiratory disorders. Basic scientific discoveries in the past year have included improved disease modelling and in vitro correction of some monogenic chILD disorders. In the clinical domain, multicentre collaborative studies have been initiated to explore shared clinical, radiologic and histologic features of chILD cohorts, and biomarkers for some chILD disorders have recently been identified. There is also increasing recognition of chILD associated with rheumatological and immunological disease. In a major advance for the treatment of chILD, which currently remains limited and non-specific, a randomised, clinical trial (NCT04093024) of nintedanib for paediatric patients with fibrosing ILD has now been initiated and will collect detailed clinical data on both disease natural history and the impact of intervention.
Clinical Year in Review of ILD
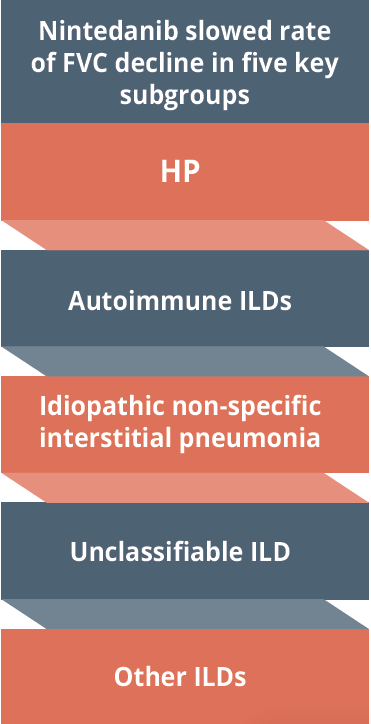
The efficacy of nintedanib in reducing annual rate of decline in forced vital capacity is maintained across five key subgroups
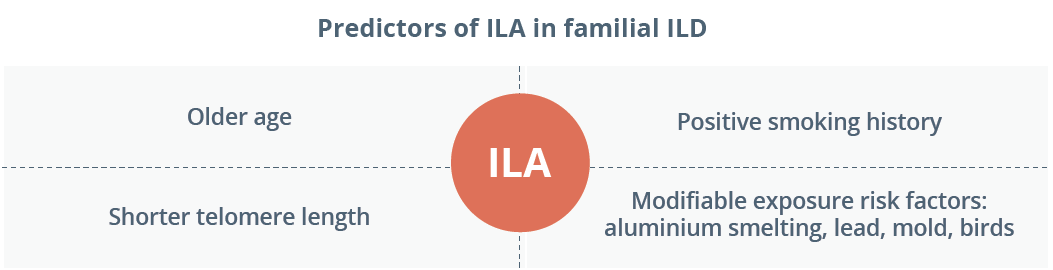
Julie Morisset, Montreal, Canada, highlighted five key papers in ILD from the past year. The first was new clinical practice guidelines from ATS/JRS/ALAT on the diagnosis of HP in adults, which recommend consideration of HP in the differential diagnosis of all ILD cases. Two further studies focused on familial ILD and pinpointed key predictive factors for the development and progression of interstitial lung abnormalities (ILA) in at-risk individuals. Dr Morisset also drew attention to subgroup analysis from the INBULD trial (NCT02999178) which has confirmed that the efficacy of nintedanib in reducing annual rate of decline in forced vital capacity (FVC; ml/year) is maintained across all five groups of ILD diagnosis. Finally, Dr Morisset discussed findings from a UK observational study looking at persistent inflammatory ILD after admission for COVID-19-pneumonia. In total, 395 patients (39%) had persistent symptoms and 59 showed post-COVID interstitial changes, most commonly radiological features suggestive of organising pneumonia.
Closing Remarks
Looking ahead to next year’s congress, ATS is planning a live, in-person event in San Francisco which will be complemented by a rich array of online content. This hybrid conference will take place in May 2022, with final dates to be confirmed.
©Springer Healthcare 2021. This content has been independently selected and developed by Springer Healthcare and licensed by Roche for Medically. The topics covered are based on therapeutic areas specified by Roche. This content is not intended for use by healthcare professionals in the UK, US or Australia. Inclusion or exclusion of any product does not imply its use is either advocated or rejected. Use of trade names is for product identification only and does not imply endorsement. Opinions expressed do not reflect the views of Springer Healthcare. Springer Healthcare assumes no responsibility for any injury or damage to persons or property arising out of, or related to, any use of the material or to any errors or omissions. Please consult the latest prescribing information from the manufacturer for any products mentioned in this material.