
The 2020 annual International Congress of the European Respiratory Society (ERS) was held as an interactive virtual event. The ERS used the latest technology to join together over 33,000 delegates from around the world. In the midst of the current COVID-19 pandemic, the ERS were determined that the congress should still take place as it could be more important than ever to connect the respiratory community, share data and to provide educational opportunities.


An overview of sessions and attendees at ERS 2020
Welcome to ERS 2020
The President of ERS, Thierry Troosters, Leuven, Belgium, hoped that the digital format of the congress would provide an opportunity for people from all around the globe to connect in large numbers. He anticipated it would provide fertile ground to exchange ideas to move respiratory health forward into the next decade. Hot topics include the relationship between exercise, physical activity and sleep quality and the increasing role of digital interfaces to support patients in between face-to-face appointments.
Cystic fibrosis
Cystic fibrosis (CF) is a severe, chronic, progressive, multi-organ disease caused by mutations in the CF transmembrane conductance regulator gene (CFTR). CF was the focus for a large number of sessions during this year’s ERS congress.
Clinical and translational challenges in patient care
The educational symposium, ‘Cystic Fibrosis: From Cradle to Old Age’, aimed to describe the major clinical and translational challenges in caring for patients with CF in the 21st century, and to describe the pathophysiology and clinical characteristics of CF.
Historically, there has been a focus on the identification and eradication of bacterial pathogens as the cause of inflammation in CF but Stephen Stick, Perth, Australia, presented the case for inflammation being a precursor to infection. It has been shown that airway inflammation begins in early infancy with increased neutrophil elastase, interleukin (IL)-8 and neutrophils detected in bronchoalveolar lavage (BAL) samples at 3 months. Computerised tomography (CT) scans show that these inflammatory changes correspond with progressive lung damage. Recent data from the Australian Respiratory Early Surveillance Team for Cystic Fibrosis (AREST CF) programme found very low pathogen load in BAL samples from children with CF despite high levels of inflammation. Specifically, muco-obstructive inflammation is the trigger for early lung damage and is associated with a neutrophil phenotype characterised by exocytosis. Improving the understanding of these pathological mechanisms presents more potential targets for treatment with CF transmembrane conductance regulator (CFTR) modulators. Targets include antiproteases, trefoil factors, IL-1 pathway and airway dehydration. There are some recent data that suggest CTFR modulators might mitigate muco-obstructive inflammation but more work is required to determine whether CFTR modulators can reduce inflammation.
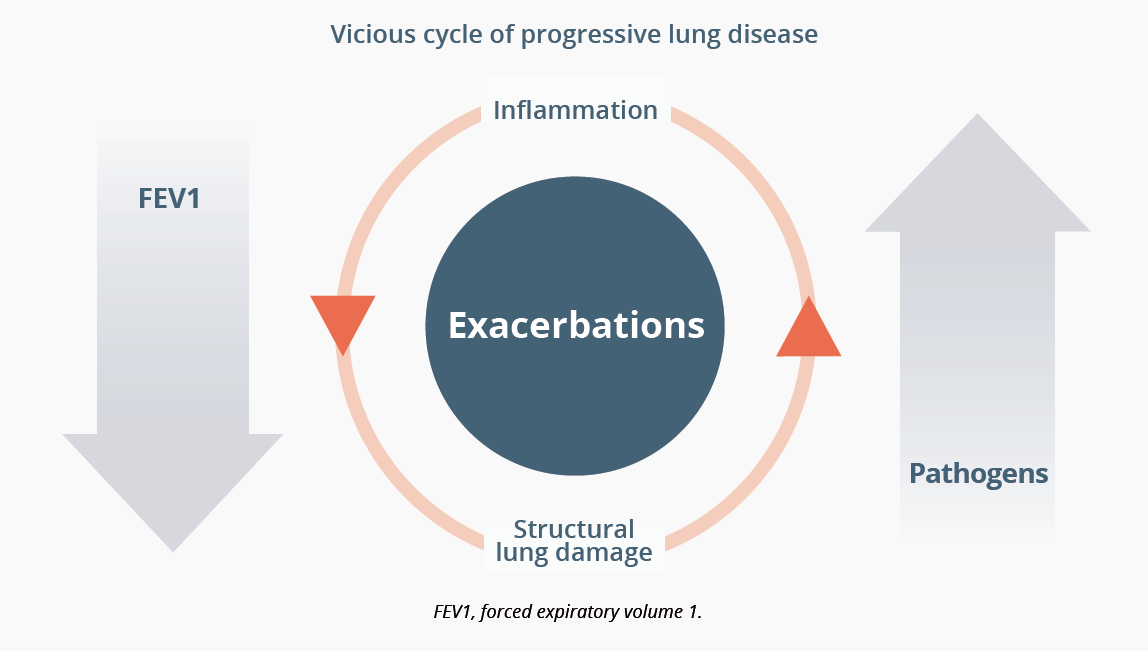
In a related talk on the previous day, Professor Stick, Perth, Australia, also showed how inflammation from a young age can predict lung damage and exacerbations in a vicious cycle. There is a steady decline in lung function along with a gradual accumulation in pathogenic bacteria, all modified by exacerbations and the random nature of gene modifiers.
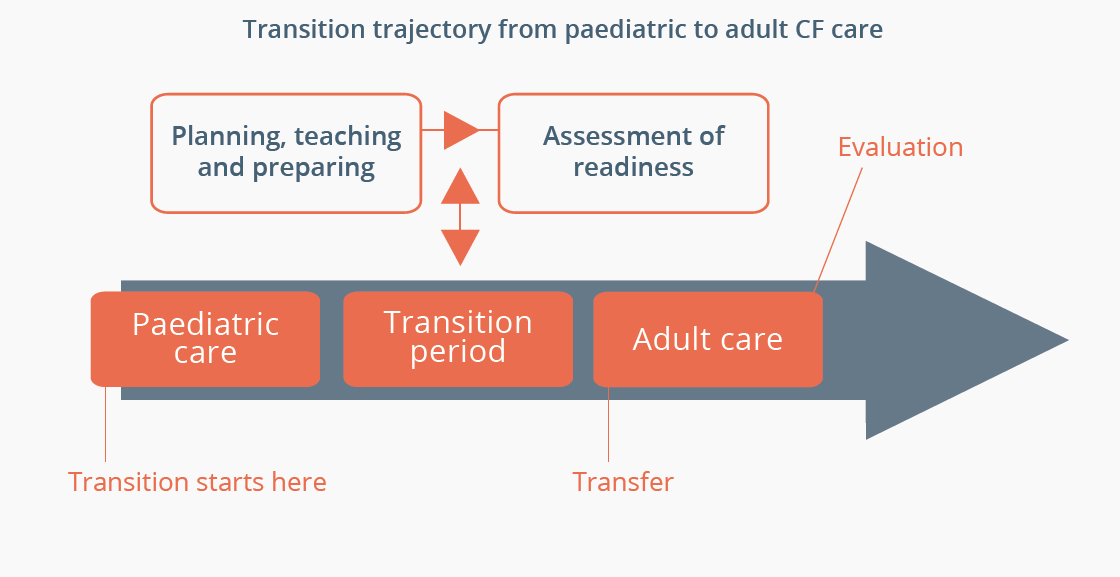
An important issue when considering the lifelong pathway of a patient with CF is to successfully manage the transition from paediatric to adult care. The focus and nature of these two types of clinic by definition are very different to one another, with the paediatric clinic being a protective, nurturing, family-orientated environment for development and growth while the adult clinic aims to give the patient autonomy and covers adult issues. In her presentation, Trudy Havermans, Leuven, Belgium, reviewed the typical obstacles of fear and mistrust that can arise from the children/parents, paediatrician and adult physician when moving from the paediatric to the adult clinic as well as practical issues such as lack of time and reimbursement. These issues can be addressed in a well-developed transition programme that includes joint consultations between the patient and both the paediatric and adult counterpart healthcare practitioner, including pre-transition visits to the adult centre. Communication between paediatric and adult teams is critical for success.
“There is no defined age for transition from paediatric to adult services but ideally patients should begin a transition programme between 12 and 18 years of age with transition complete by 20 years.”
- Trudy Havermans, Leuven, Belgium
Barry Plant, Cork, Ireland, highlighted the importance of the microbiota of the gut and its relationship with health in CF. Previous studies have demonstrated that lower diversity of gut bacteria is associated with poorer health. Furthermore, certain bacterial assemblages appear in the gut prior to CF respiratory complications. Professor Plant presented new data from the CF Microbiome-determined Antimicrobial Therapy Trial in Exacerbations (CF MATTERS; NCT02526004) in which they collected data from gut microbiota. Analysis revealed patterns of dominance of certain bacteria among the patients with CF compared with healthy controls and this correlated with CF phenotypes. The relationship between gut microbiota and the lungs remains to be defined by further studies but there may be a role for probiotics in CF.
With the advances in CF care over recent decades, life expectancy has improved substantially and over 50% of patients born today are expected to live beyond the age of 50. UK registry data predict that by 2030 the majority of patients with CF will be 30–45 years old with survival possible beyond 90 years. In addition to increased prevalence of CF-related comorbidities such as diabetes, depression, bone disease and joint problem, patients’ increased longevity means that they are also at risk of traditional age-related comorbidities such as cardiovascular disease (CVD). Josje Altenburg, Amsterdam, Netherlands, explained that patients with CF will be exposed to both CF-related and traditional risk factors for CVD. Because of their condition, patients with CF are on a high-fat diet. Furthermore, exposure to constant infection leads to systemic inflammation, oxidative stress and endothelial dysfunction. Measures to prevent CVD in older patients with CF should target both CF-related and traditional risk factors. In addition, a cardioprotective high-fat diet (mono- and poly-unsaturated fats) should be encouraged, as well as performing a yearly check of lipid profile, discouraging smoking and treating obesity.
“CVD in CF will become more common in the future.”
- Josie Altenburg, Amsterdam, Netherlands
Treatment considerations for patients with CF

The underlying cause of CF is the loss of epithelial chloride transport due to over 2000 identified mutations in the CFTR gene that encodes the CFTR protein. CFTR mutations cause a loss of chloride transport through CFTR that results in the accumulation of thick, sticky mucus in the bronchi of the lungs, exocrine pancreatic insufficiency, impaired intestinal absorption, reproductive dysfunction and elevated sweat chloride concentrations. Felix Ratjen, Toronto, Canada, discussed the clinical implications of CFTR modulators and concluded that they have changed the treatment landscape for patients living with CF. These CFTR-directed therapies can either be correctors to overcome folding defects within the protein, or potentiators to facilitate the chloride transport at the channel. The most common mutation is F508del and this can be treated with a CFTR potentiator. Although the combination of CFTR correctors and potentiators has a marked benefit on lung function and improves the microbiome, chronic infection has been shown to persist. Observational studies are in progress that will clarify whether infection can be prevented with early therapy.
Recent breakthroughs around potentiators and correctors were also discussed in an educational symposium about the European Reference Network for rare lung diseases (ERN-LUNG). Marcus Mall, Berlin, Germany, explained that it was the realisation that the common F508del mutation causes not single but multiple folding defects which led to the development of next-generation CFTR correctors, such as elexacaftor, and their combination with existing CFTR modulators.
Professor Mall presented preclinical data in which elexacaftor added to tezacaftor and ivacaftor results in increased CFTR function in vitro. In addition, Professor Mall presented two recent Phase III clinical trials (NCT03525444 and NCT03525548) that showed the preclinical findings translated to improvements in lung function and exacerbation rate in patients with CF with F508del. Triple therapy leads to unprecedented improvement in CFTR function and clinical benefits in up to 90% of patients who carry at least one F508del allele.
“These highly-effective CFTR-directed therapeutics may transform CF from a fatal disease to a treatable chronic condition.”
- Marcus Mall, Berlin, Germany
Christian Benden, Berne, Switzerland, agreed that the overall survival in individuals with CF continues to improve and the introduction of CFTR modulator therapies may even provide benefit in patients with advanced CF lung disease. Every patient with CF who is applicable for new treatment will undergo a treatment trial. However, if no other medical or surgical therapy option is available, lung transplantation is the standard-of-care in patients with progressive lung disease, according to guidelines from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation (ISHLT). CF is the most common indication for lung transplantation in children and is the third most common reason in adults. Professor Benden presented recent data from the ISHLT Thoracic Transplant Registry showing that patients with CF are receiving lung transplants at an older mean age compared with previous decades. Overall median survival after transplantation continues to improve and is currently over 9 years. However, Professor Benden noted a worrying trend of lower survival in teenage patients associated with a poor adherence to treatment.
“No individual with CF should nowadays die without consideration for lung transplantation.”
- Christian Benden, Berne, Switzerland
Microbiome and antibiotic research
Thomas Bjarnsholt, Copenhagen, Denmark, calculated that at the end of one of his patient’s 28-year-life, the patient had consumed 1 kg of tobramycin, 10 kg of beta-lactam anti-pseudomonas antibiotics and 1 kg of inhaled colistin. While long-term treatment with antibiotics can be helpful in delaying disease progression, it fails to eradicate the bacteria that reside in the thick mucus within the respiratory tissue. Using biofilms to study the antibiotic resistance of these bacteria is challenging because the in vitro microenvironment is different to the human infection in vivo. Bacterial cells being attached to a flat surface versus suspended within mucus leads to marked differences in perfusion of oxygen and penetration of antibiotics. Interestingly, data suggest that bacteria develop tolerance to antibiotics in hypoxic microenvironments and become more susceptible to treatment when they have more oxygen. Further research is required on this topic of promotion of growth to increased susceptibility.
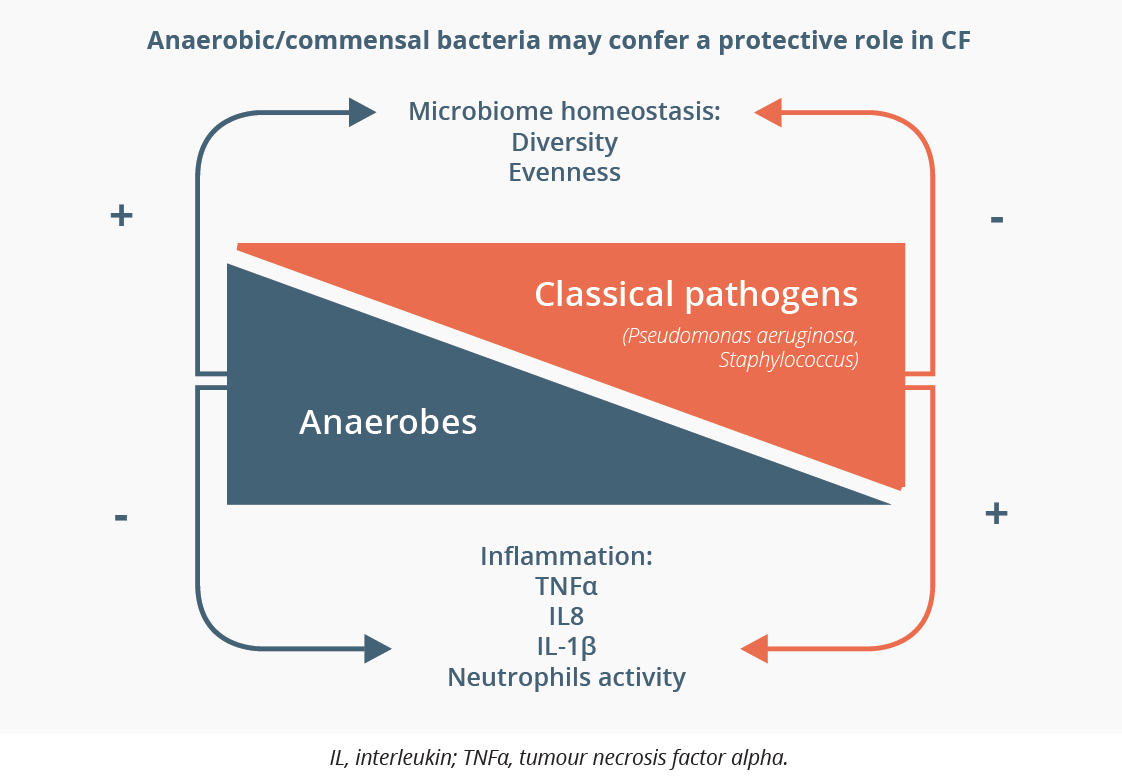
Alexander Dalpke, Dresden, Germany, presented data on bacterial dysbiosis (a disturbance of the composition of microbial communities) in the CF lung, and how this correlates to clinical outcome. Professor Dalpke observed that there are clusters of patients who have dominance of particular bacteria, like Pseudomonas aeruginosa, Streptococcus or Staphylococcus, while others show a diverse mixture of bacteria. Microbiome diversity, particularly where anaerobic bacteria are included, is correlated with better lung function and reduced inflammation whereas dominance of a single strain is associated with worse function. The most recent data suggest that commensal bacteria, i.e. those that grow alongside one another, can inhibit the growth of typical lung pathogens.
Digital health
Vitalii Poberezhets, Vinnytsia, Ukraine, discussed new horizons in digital technologies for respiratory medicine based on an ERS literature update of forty-eight publications. Artificial intelligence (AI) and machine learning are increasingly being used in respiratory medicine for thoracic imaging, histopathology and cytology. These technologies can help ease the workload of radiologists and reduce the chance of missing a diagnosis. Digital technologies are also being applied to Clinical Decision Support Systems that allow individuals to seek advice based on their symptoms. Other applications of digital technologies that can support the interaction between healthcare professionals and patients include telerehabilitation, telemonitoring and teleconsultation.
Konstantinos Kostikas, Ioannina, Greece, explained that AI techniques are likely to have a role in the running of future clinical trials in respiratory medicine. AI has the potential to transform clinical trial design, in all steps from study preparation to execution, including feasibility, patient identification and matching, real-time monitoring of patients and centres, and generation of the study report. A key benefit will be to improve enrichment to select patients more likely to show measurable clinical endpoints.
Closing Remarks
The next ERS International Congress will be held in Barcelona, Spain from 4–8 September 2021.
©Springer Healthcare 2020. This content has been independently selected and developed by Springer Healthcare and licensed by Roche for Medically. The topics covered are based on therapeutic areas specified by Roche. Inclusion or exclusion of any product does not imply its use is either advocated or rejected. Use of trade names is for product identification only and does not imply endorsement. Opinions expressed do not reflect the views of Springer Healthcare. Springer Healthcare assumes no responsibility for any injury or damage to persons or property arising out of, or related to, any use of the material or to any errors or omissions. Please consult the latest prescribing information from the manufacturer for any products mentioned in this material.